Diarrhea is one of the most common reasons for people to visit their doctor. However, it is not always necessary to treat diarrhea using medication. Nevertheless, micronutrient medicine can provide a valuable contribution. It promotes recovery and eases the symptoms, especially in the case of persistent chronic diarrhea. The article provides you with an overview of which nutrients are particularly effective when suffering from diarrhea.

Causes and Symptoms
What is diarrhea and what are the symptoms?
Doctors characterize diarrhea as when someone has a bowel movement more than three times a day and the texture of the stool is loose, i.e. watery or even liquid. It is also common for the amount of stool expelled to be more than normal. Depending on the cause of the diarrhea, there may be other symptoms such as abdominal pain, fever, flatulence, nausea, or vomiting.
Depending on how the condition progresses, doctors differentiate between acute diarrhea, lasting only a few days, and chronic diarrhea. Chronic diarrhea is when the illness lasts more than 14 days and will usually require further assessment by a doctor. Visit your doctor if the episodes of diarrhea last more than three days. Special care should be taken when babies, small children, and older people are suffering from diarrhea. The extreme loss of fluid and electrolytes can cause dehydration and place the circulatory system under extreme pressure. In severe cases, the patient can suffer a drop in blood pressure, circulation problems, and impaired consciousness, and even coma.
Tips
Seek medical advice iif you have diarrhea and a temperature of over 38 °C or you notice blood in your stool. Diarrhea can pose a risk for people who are taking daily medication. The diarrhea does not allow the medication to be fully absorbed by the intestines and therefore reduces its effectiveness. Ask you doctor what you need to consider when taking medication during an episode of diarrhea.
What are the causes of diarrhea?
The most prominent causes of acute diarrhea include food poisoning and gastrointestinal infections (gastroenteritis). These are triggered by the presence of certain types of bacteria, viruses or intestinal fungi. In bacterial infection, the cause can either be the pathogen itself or the toxins it produces. These toxins can cause inflammation of the intestinal mucous membrane and impair intestinal function.
Tips
To avoid food poisoning, ensure that you thoroughly wash fruit and vegetables and that animal products, such as eggs or chicken, are well-cooked. Most bacteria are neutralized at temperatures between 70 to 100 °C. Easily perishable foods, such as milk and meat, should always be stored in the refrigerator.
Certain types of medications, such as chemotherapeutic drugs or antibiotics, can have a negative impact on the intestinal flora. Psychological factors like stress, anxiety, and excitement can also over-activate the digestive system.
The underlying cause of chronic diarrhea is often intolerance to certain types of food. These include gluten intolerance (celiac disease), dairy product intolerance (lactose intolerance), and fructose intolerance. Examples of organic illnesses which can cause diarrhea include chronic-inflammatory intestinal diseases such as Crohn's disease or ulcerative colitis, bowel cancer, hyperthyroidism or irritable bowel syndrome.
Aim of the treatment
What is the standard treatment for diarrhea?
The principle goal in the treatment of diarrhea is to normalize the fluid and electrolyte levels in the body and to relieve the acute symptoms.
You should therefore drink plenty of fluids. Lightly-sweetened teas and diluted fruit juices are good options. The high sugar content of pure fruits juices and lemonades can intensify the symptoms and therefore should be avoided. Due to its low levels of salts, tap water is also not recommended. Salted soups and crackers are good options. When suffering from diarrhea, a low-fat and easily digestible diet is recommended with filling foods such as rice, banana, or rusks.
If deemed severe, your doctor will prescribe medication to treat the diarrhea:
- Peristalsis inhibitors help reduce intestinal over-activity and reduce the need to go to the bathroom. The active substance loperamide is a particularly effective example of this (for example, Imodium® and Lopedium®, and Lopermide HCI®).
- Antiemetics are prescribed to treat diarrhea with vomiting. They act against nausea and the urge to vomit. Antiemetic active substances include dimenhydrinate (for example, Dramamine®), domperidone (for example, Motilium®) or metoclopramine (for example, Reglan®).
- Antibiotics are only effective against diarrhea in certain cases, for example, for those with weakened immune systems or when there is blood in the stool. The prerequisite is that the diarrhea was triggered by a bacterial infection, as antibiotics are only effective against bacteria.
Tips
Ensure adequate hygiene: The pathogens are often highly contagious. Effective hygienic measures include washing your hands after going to the bathroom, before preparing food and following contact with objects which may be contaminated with the pathogen (for example, diapers, door handles, and sinks).
The aims of micronutrient medicine
Micronutrient medicine helps normalize the fluid and electrolyte levels and relieves the symptoms of diarrhea:
- Minerals like magnesium, potassium, and zinc help replace the massive loss of electrolytes.
- Health-promoting intestinal bacteria (probiotics)and their nutrients (prebiotics) help restore the imbalanced intestinal flora.
- Certain medicinal plants and their active substances, for example, chamomile, quercetin, rutin, green tea extract or curcuma help counteract intestinal irritation, protect the intestines from oxidative stress, and strengthen the immune system.
Especially in cases of chronic diarrhea, special care must be taken to avoid vitamin and mineral deficiencies. In these cases, micronutritionists will commonly recommend a multicompound product with all important vitamins and minerals – for example, all B vitamins, alongside vitamins which are important for the immune system, such as vitamins C and D.
Treatment using micronutrients
Probiotics help restore balance to the intestinal flora
How do probiotics work?
The intestines contain large amounts of microorganisms which are known collectively as intestinal (gut) flora. Diarrhea is often the result of an imbalanced intestinal flora.
Probiotics help regulate the intestinal flora. Probiotics contain microorganisms, for example, lactic acid bacterias (lactobacillus) or yeasts (for example, saccharomyces boulardii). These colonize and promote the regeneration of healthy intestinal flora: They help strengthen immune responses, fight against foreign bacteria, and promote health and the permeability of the intestinal wall. Therefore, experts and professional societies recommend the use of probiotics to treat acute diarrhea. Numerous studies have confirmed their positive effects:
Acute infectious diarrhea: Several major reviews which analyzed the data from scientific studies concluded that probiotics can reduce the duration of acute diarrhea by one day. The number of bowel movements was also rapidly reduced. Children with gastroenteritis also benefited from shorted hospital stays.
Prevention: If you suspect that you will soon be suffering from traveler's diarrhea or infectious diarrhea, the preventive application of probiotics is recommended. An overview of available medical studies concluded that the use of probiotics reduced the cases of traveler's diarrhea by between six and 21 percent. Also, the overall risk for diarrhea of different causes was reduced by 34 percent.
Non-infectious diarrhea: People with chronic-inflammatory bowel diseases or irritable bowel syndrome who develop diarrhea will also most likely benefit from the use of probiotics: Initial study findings have shown that treatment with probiotics improves the barrier functions of the intestinal tract and can ease symptoms. However, further high-quality studies are required to confirm this effect.
Probiotic treatment has very few side-effects, making it very safe for adults and children alike.
Dosage and recommended use of probiotics
Suitable amounts are required to ensure that a sufficient number of the live bacteria arrive in the gut. Doctors recommend an intake of at least one billion (109), or ideally 10 to 20 billion (2 x 1010) bacteria per day. They are measured in Colony Forming Units (CFU). Lactobacilli, bifidobacteria, escherichia coli, and the yeast saccharomyces boulardii are particularly recommended.
Probiotics are best taken during mealtimes or with plenty of fluids. Tablets or capsules can be taken with water, while powdered product can be mixed with water, milk or yogurt. It is important that the bacteria are taken over an extended period of time.
Instructions if taking antibiotics or during illness
Very weak patients with suppressed immune systems, persons with a central venous catheter, heart valve disease, or short bowel syndrome, along with premature babies, should not use probiotics.
If you are taking antibiotics, leave a period of at least two hours between taking the antibiotics and taking probiotics: Antibiotics kill the beneficial intestinal bacteria along with the harmful bacteria.
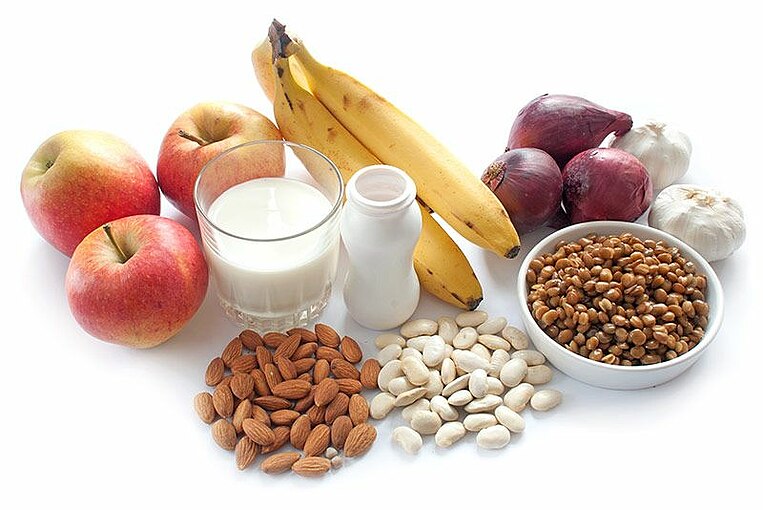
Prebiotics act as food for the intestinal flora and inhibit intestinal inflammation.
How do prebiotics work?
Most prebiotics are carbohydrates which remain undigested in the intestine (fiber). Prebiotics act as food for the intestinal bacteria and help increase their activity and growth. This makes it easier for good intestinal bacteria to remove the types of bacteria which can trigger illness.
During the bacterial decomposition process, fatty acids (such as butyric acid) are produced, making the intestinal environment more acidic. This helps prevent the growth of pathogens. The fatty acids also help reduce intestinal inflammation and encourage water absorption in the large intestine. This helps them counteract diarrhea.
An example of a prebiotic is resistant starch. The positive effects of resistant starch has been shown by scientists in several small-scale studies: Resistant starch was shown to notably reduce the illness duration in men with cholera-like diarrhea, sometimes by more than half. Levels of fluid loss were also less than in the control group who had not been given resistant starch. During the study, all the participants were given a standard drinkable solution containing minerals to balance out losses. The solution (oral rehydration solution) contained, along with minerals, either dextrose or resistant starch.
In another clinical study, children given resistant starch recovered more rapidly than those who had not been given prebiotic treatment. During this study, the standard drinkable solution included minerals and resistant starch in addition to dextrose.
Dosage and recommended use of prebiotics:
As a supportive treatment for diarrhea, approx. 25 grams of resistant starch per day is recommended, taken at mealtimes throughout the day. Dissolve the powder in cold or warm fluid, for example, a glass of water, in soup or broth.
Initially, resistant starch can cause flatulence (wind) in more sensitive patients. Therefore, it is recommend to slowly increase the dosage and to begin with one third of the daily dosage, eight grams. When you feel that you are able to tolerate this amount that you can double the dosage.
Sodium, Potassium, Calcium, Magnesium and Zinc: Replacing lost minerals
How do minerals work?
Diarrhea causes the body to lose not only fluids, but also large amounts of minerals. It is therefore vital to replace these lost minerals. This can be a major problem with persistent diarrhea. It can also lead to life-threatening conditions, such as circulatory collapse. The minerals sodium, potassium, calcium, magnesium, and zinc are responsible for many important functions in the body, including water balance and thereby circulation and blood pressure.
To return mineral levels to normal, standard drinkable solutions (oral rehydrations solutions) are used. In addition to water and dextrose they also contain vital minerals.
Especially for children the World Health organization (WHO) recommends administering standard rehydration solution. Zinc reduces loss during diarrhea. Zinc also has a positive effect on the immune system and aids the regeneration of the damaged intestinal mucous membrane.
The positive effects of zinc in the treatment of diarrhea, especially in patients with a zinc deficiency, has been confirmed in studies. For example, two comprehensive high-quality studies found that the administration of zinc can reduce the duration of diarrhea in children.
Dosage and recommended use of minerals:
Acute Diarrhea: To counterbalance the loss of minerals during diahhrea, the WHO recommends a standard rehydration solution: A suitably dosed granulate (sodium, chlorine, potassium, and dextrose) is available at most pharmacies. It must be dissolved in water. For children, the WHO recommends a zinc dosage of 10 to 20 milligrams per day for 10 to 14 days.
Persistent Diarrhea: Persistent diarrhea can also cause deficiencies in other minerals. Therefore, micronutritionists recommend a compound containing all important minerals, including 100 to 150 milligrams of magnesium, 200 to 300 grams of calcium, and 300 to 500 milligrams of potassium.
Instructions if taking medications or if suffering from kidney disease
Antihypertensive medication (ACE inhibitors, for example Rampiril® or AT1 blockers such as Corzaar®) and potassium-sparing diuretics (for example, Inspra®) reduce the amount of potassium expelled from the body via the kidneys. They therefore cannot be used in conjunction with potassium supplements. Potassium can also reduce the effects of certain types of heart medications (cardiac glycosides). This includes the active compounds digitoxin (e.g., Lanoxicap®) or digoxin (e.g.,Lanoxin®). Therefore, additional potassium supplements should not be used. You can find all the relevant information regarding the interaction between potassium and medication under the section headed Potassium: Overdose, Interactions, and Illness-Related Instructions:
Zinc can bind with osteoporosis (bisphosphonate) medication and render it ineffective. There, it is recommended to leave at least two hours between taking each substance. Examples of this types of medication are gyrase inhibitors, such as Ciprofloxacin (e.g., Ciloxan®), tetrayclines (e.g., Sumycin®)nd and biphosphates such as alendronic acid (e.g., Fosamax®).
Patients suffering from kidney diseases should not use magnesium, potassium, calcium, or zinc supplements. Impaired kidneys are not able to fully excrete excess minerals.
Chamomile has a calming effect on the intestinal tract.
How does chamomile work?
Chamomile has several characteristics which have positive effects on the intestinal tract and stomach when suffering from diarrhea. Chamomile has an anti-inflammatory, antispasmodic and antibacterial effect. Even though chamomile has been used as a medicinal plant for centuries, the use of chamomile is usually based on experience.
Tests carried out in animals have demonstrated the use of chamomile in the treatment of diarrhea: Chamomile may - like active substance loperamide - help relieve diarrhea, cramps, and the collection of fluid in the abdomen. Diarrhea also appears to be associated with increased oxidative stress, which can be relieved by chamomile.
The positive effects of combination products containing chamomile have been proven: In a preliminary study, a product containing myrrh, coffee charcoal, and chamomile reduced the symptoms of diarrhea. The effectiveness of the product was comparable with other conventional products for the treatment of diarrhea. A high-quality study with children produced similar findings: Patients who were given treatment with chamomile and pectin (dietary fibers) recovered far quicker that those given a placebo.
Dosage and recommended use of chamomile:
Micronutritionists recommend the use of chamomile extract because this has higher levels of active ingredients than powder or tea, for example. Chamomile is effective in the treatment of diarrhea at a dosage of between 70 and 300 milligrams per day.
Instructions during pregnancy or when breastfeeding
As there are currently insufficient studies available on the use of chamomile during pregnancy and when breastfeeding, please consult your doctor.
Quercetin and rutin can relieve the symptoms of intestinal inflammation
How do quercetin and rutin work?
The secondary plant substances (phytochemicals) quercetin and rutien are closely related to one another. There are said to have extensive antioxidant characteristics: They are able to detoxify aggressive oxygen-based free radicals. Both plant substances also have anti-inflammatory characteristics which inhibit the release of inflammatory messenger substances. Quertin was also shown to have antibacterial properties which are effective against almost all types of bacteria. It also increases the protective barrier function of the intestine, which helps relieve the symptoms of diarrhea and can reduce the uptake of toxins and contaminants.
The effects of quercetin and rutin were mainly examined in laboratory and animals tests to determine their effectiveness in the treatment of inflammatory intestinal disorders. Quercetin is most active in the small intestine, and rutin in the large intestine.
No clinical studies on humans have been carried out. Initial reviews have shown that the intake of quercetin can significantly reduce the concentration of an important inflammatory value in humans, the C-reactive protein value. This enables the body to recover quicker from intestinal inflammation.
Dosage and recommended use of quecetin and rutin:
Quercetin is generally applied at a dosage of up to 500 milligrams per day. For diarrhea, the recommended rutin dosage is 25-50 milligrams per day.
Rutin and quercetin should be taken at mealtimes with sufficient amounts of fluid. This helps the stomach better tolerate the substances. Initial clinical studies have shown that fats in our diet improve the body's absorption of quercetin.
EGCG: Green tea protects against infection and reduces intestinal inflammation
How does EGCG work?
EGCG (Epigallocatechin gallate) is the main active substance in green tea and has pronounced anti-inflammatory properties and antioxidative effects, which develops mainly in the large intestine. It can also help protect the body against certain types of viruses, bacteria, and fungi.
Initial studies have investigated the effectiveness of EGCG in the treatment of inflammatory bowel diseases. A small, but high-quality human study indicates that the active ingredient can keep the disease at bay and alleviate symptoms. However, high dosages should be avoided.
No studies on its effectiveness in the treatment of diarrhea have yet been carried out, but it is suspected to have a positive effect. Traditional medicine in Asia uses green tea as a treatment for diarrhea.
Dosage and recommended use of EGCG:
At a dosage of between 400 and 800 milligrams per day, ECHC can help reduce the symptoms of inflammatory intestinal disorders. Micronutritionists recommend taking an extract because it contains an exactly specified amount of the active ingredient.
Always take tablets or capsules containing green tea extract with fluid at mealtimes to improve tolerability.
Instructions during pregnancy, breastfeeding, in patients with liver disease or if taking medication
Certain substances found in green tea block the intestinal absorption of active substances, such as the betablocker Bisoprolol (e.g., Bisoprolol®, Concor®), or the antihypertensive medication Nifedipin (Adalat CC, Afeditab CR, and Procardia XL). Between doses there should therefore be a period of at least two hours.
If you are suffering from liver problems, or if there is a history of liver problems in your family, consult your doctor beforehand and ask him to carry out any necessary tests.
There are no studies examining the use of green tea extract during pregnancy, of when breastfeeding. Therefore, pregnant women and mothers who are breastfeeding should not use green tea extract. The use of green tea in children under 18 years of age has also not been studied sufficiently, and so a doctor should decide on the use of green tea supplements.
Dosage overview
Daily micronutrient recommendation for diarrhea | |
|---|---|
Probiotics and dietary fibers | |
Probiotics with lactobacilli and saccharomyces boulardii yeast | 1 to 20 billion (109 to 2 x 1010) Colony Forming Units (CFU) |
Resistant starch | up to 25 grams (g) |
Minerals | |
Calcium | 200 to 300 milligrams (mg) |
Magnesium | 100 to 150 milligrams |
Potassium | 300 to 500 milligrams |
Zinc | 10 to 20 milligrams (for children) |
Plant substances | |
Chamomile extract | 70 to 300 milligrams |
Quercetin | up to 500 milligrams |
Rutin | 25 to 50 milligrams |
EGCG | 400 to 800 milligrams |
Supporting the effects of medication with micronutrients
Probiotics during and after antibiotic treatment.
In indicated cases, diarrhea may be treated using antibiotics. However, antibiotics also kill the beneficial intestinal bacteria along with the harmful bacteria. This can cause long-term harm to the intestinal flora and lead to persistent diarrhea, which may continue beyond the end of the antibiotic treatment.
Various high-quality studies, including an extensive review, have shown evidence that the bacteria lactobacillus rhamnosus and the yeast Saccharomyces boulardii are both able to normalize intestinal flora and relieve or even prevent the development of antibiotic-induced diarrhea. A dose of at least 1 to 20 billion (109 to 2 x 1010) colony forming units (CFU) is recommended.
It should also be noted that antibiotics can damage probiotics. It is therefore always advisable to take these substances at different times, with an interval of at least two to three hours.
Dosage overview
Daily micronutrient dosage recommendation when taking antibiotics | |
|---|---|
Probiotics with lactobacilli and saccharomyces boulardii yeast | 1 to 20 billion (109 to 2 x 1010) colony forming units (CFU) |
Summary
Diarrhea can have many causes. Usually, it is caused by infection, but intestinal illnesses, medication, food, and stress can often trigger diarrhea. The symptoms can be relieved by the use of medication. Micronutrient medical treatment can also help relieve the symptoms of diarrhea:
Probiotics and prebiotics help restore damaged intestinal flora and fight harmful bacteria. They help strengthen the barrier function of the intestinal tract, calm the irritated mucous membrane and reduce inflammation.
Minerals such as potassium, magnesium, calcium and zinc are important to replace the extensive loss of minerals as a result of the diarrhea. These minerals are essential for the water balance in the body, for the correct functioning of nerve and muscle cells, for the circulation and blood pressure, the energy metabolism, and the immune system.
Plant substances such as chamomile, quercetin and ECCG, from green tea, have anti-inflammatory and antibacterial properties. They also have antioxidative characteristics and protect the intestinal tract from the harmful effects of free oxygen radicals.
In the event that a course of antibiotics are prescribed to treat diarrhea which is the result of bacterial infection, it is important to boost intestinal health by supplementing with probiotic bacteria: Probiotics restore balance to the intestinal flora and prevent antibiotic-induced diarrhea.
Study and Source Index
Ahmadi, E. et al. (2015): Efficacy of probiotic use in acute rotavirus diarrhea in children: A systematic review and meta-analysis. Caspian J Int Med. 2015; 6(4): 187-95. https://www.ncbi.nlm.nih.gov/pubmed/26644891, retrieved on: 2018-07-04.
Albrecht, U. et al. (2014): Efficacy and safety of a herbal medicinal product containing myrrh, chamomile and coffee charcoal for the treatment of gastrointestinal disorders: a non-interventional study. BMJ Open Gastroenterol. 2014; 1(1): e000015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533328/, retrieved on: 2018-07-04.
Allen, S.J. et al. (2010): Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2010; (11):CD003048. doi: 10.1002/14651858.CD003048.pub3. https://www.ncbi.nlm.nih.gov/pubmed/21069673, retrieved on: 2018-07-04.
Arastéh, K. et al. (2013): Innere Medizin. 3. Aufl. Thieme Verlag Stuttgart.
Bajait, C. und Thawani, V. (2011): Role of zinc in pediatric diarrhea. Indian J Pharmacol. 2011: 43(3): 232-5. https://www.ncbi.nlm.nih.gov/pubmed/21713083, retrieved on: 2018-07-04.
Becker, B. et al. (2006): Double-blind, randomized evaluation of clinical efficacy and tolerability of an apple pectin-chamomile extract in children with unspecific diarrhea. Arzneimittelforschung. 2006; 56(6): 387-93. https://www.ncbi.nlm.nih.gov/pubmed/16889120, retrieved on: 2018-07-04.
Biesalski, H.-K. (2016): Vitamine und Minerale. Indikation, Diagnostik, Therapie. Georg Thieme Verlag Stuttgart New York.
Biesalski, H.-K. et al. (2010): Ernährungsmedizin. 4. Aufl. Georg Thieme Verlag Stuttgart.
Binder, H.J. et al. (2014): Oral rehydration therapy in second decade of the twenty-first century. Curr Gastroenterol Rep. 2014; 16(3): 376. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3950600/, retrieved on: 2018-07-04.
Bischoff, S.C. et al. (2009): Probiotika, Präbiotika und Symbiotika. Thieme Verlag, Stuttgart.
Bitzer, Z.T. et al. (2016): (-)-Epigallocatechin-3-gallate decreases colonic inflammation and permeability in a mouse model of colitis, but reduces macronutrient digestion and exacerbates weight loss. Mol Nutr Food Res. 2016; 60(10): 2267-74. https://www.ncbi.nlm.nih.gov/pubmed/27218415, retrieved on: 2018-07-04.
Brückner, M. et al. (2012): Green tea polyphenol epigallocatechin-3-gallate shows therapeutic antioxidative effects in a murine model of colitis. J Crohns Colitis. 2012; 6(2): 226-35. https://www.ncbi.nlm.nih.gov/pubmed/22325177, retrieved on: 2018-07-04.
Bundeszentrale für gesundheitliche Aufklärung (BzGA): Küchen- und Lebensmittelhygiene. https://www.infektionsschutz.de/hygienetipps/kuechen-und-lebensmittelhygiene/#c6494, retrieved on: 2018-07-04.
Bundy, R. et al. (2004): Turmeric extract may improve irritable bowel syndrome symptomology in otherwise healthy adults: a pilot study. J Altern Complement Med. 2004; 10(6): 1015-8. https://www.ncbi.nlm.nih.gov/pubmed/15673996, retrieved on: 2018-07-04.
Cai, J. et al. (2018): Comparative efficacy and tolerability of probiotics for antibiotic-associated diarrhea: Systematic review with network meta-analysis. United European Gastroenterol J. 2018; 6(2): 169-80. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5833232/, retrieved on: 2018-07-04.
Castagliuolo, I. et al. (1999): Saccharomyces boulardii protease inhibits the effects of Clostridium difficile toxins A and B in human colonic mucosa. Infect Immun. 1999; 67(1): 302-7. https://www.ncbi.nlm.nih.gov/pubmed/9864230, retrieved on: 2018-07-04.
Chacko, S. M. et al. (2015): Beneficial effects of green tea: A literature review. Chin Med. 2010; 5: 13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2855614, retrieved on: 11.07.2018.
Conteas, C.N. et al. (2009): Treatment of HIV-associated diarrhea with curcumin. Dig Dis Sci. 2009; 54(10): 2188-91. https://www.ncbi.nlm.nih.gov/pubmed/19051018, retrieved on: 2018-07-04.
Cook, S.I. und Sellin, J.H. (1998): Review article: short chain fatty acids in health and disease. Aliment Pharmacol Ther. 1998; 12(6): 499-507. https://www.ncbi.nlm.nih.gov/pubmed/9678808, retrieved on: 2018-07-04.
David, A.V.A. et al. (2016): Overviews of biological importance of quercetin: a bioactive flavonoid. Pharmacogn Rev. 2016: 10(20): 84-89. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5214562/, retrieved on: 2018-07-04.
de la Motte, S. et al. (1997): Double-blind comparison of an apple pectin-chamomile extract preparation with placebo in children with diarrhea. Arzneimittelforschung. 1997: 47(11): 1247-9. https://www.ncbi.nlm.nih.gov/pubmed/9463302, retrieved on: 2018-07-04.
de Vrese, M. und Marteau P.R. (2007): Probiotics and prebiotics: effects on diarrhea. J Nutr. 2007: 137(3 Suppl 2): 803S-11S. https://www.ncbi.nlm.nih.gov/pubmed/17311979, retrieved on: 2018-07-04.
Deutsche Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselerkrankungen (2018): S3-Leitlinie – Colitis ulcerosa. Mai 2018, AWMF-Registernummer 021-009. https://www.awmf.org/uploads/tx_szleitlinien/021-009l_S3_Diagnostik_Therapie_Colitis_ulcerosa_2018-05.pdf, retrieved on: 5.7.2018.
Dinlevici, E.C. et al. (2012): Effectiveness and safety of Saccharomyces boulardii for acute infectious diarrhea. Expert Opin Biol Ther. 2012; 12(4): 395-410. https://www.ncbi.nlm.nih.gov/pubmed/22335323, retrieved on: 2018-07-04.
Dinlevici, E.C. et al. (2013): The effect of a multispecies synbiotic mixture on the duration of diarrhea and length of hospital stay in children with acute diarrhea in Turkey: single blinded randomized study. Eur J Pediatr. 2013; 172(4): 459-64. https://www.ncbi.nlm.nih.gov/pubmed/23239048, retrieved on: 2018-07-04.
Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin: S1-Leitlinie Akuter Durchfall. AWMF-Registernr. 053/030. Stand 09/2013. http://www.awmf.org/uploads/tx_szleitlinien/053-030l_S1_Akuter_Durchfall_2014-06.pdf, retrieved on: 2018-07-04.
Dryden, G.W. et al. (2013): A pilot study to evaluate the safety and efficacy of an oral dose of (-)-epigallocatechin-3-gallate-rich polyphenon E in patients with mild to moderate ulcerative colitis. Inflamm Bowel Dis. 2013; 19(9): 1904-12. https://www.ncbi.nlm.nih.gov/pubmed/23846486, retrieved on: 2018-07-04.
Ebner, J. und Gattringer, R. (2017): Bakterielle Durchfallerkrankungen. Wien Klein Wochenschr Educ. 2017; 12: 63-79. https://link.springer.com/article/10.1007/s11812-017-0083-7, retrieved on: 2018-07-04.
Freedman, S.B. et al. (2013): Treatment of acute gastroenteritis in children: an overview of systematic reviews of interventions commonly used in developed countries. Evid Based Child Health. 2013; 8(4): 1123-37. https://www.ncbi.nlm.nih.gov/pubmed/23877938, retrieved on: 2018-07-04.
Fujimori, S. et al. (2007): High dose probiotic and prebiotic cotherapy for remission induction of active Crohn's disease. J Gastroenterol Hepatol. 2007; 22(8): 1199-204. https://www.ncbi.nlm.nih.gov/pubmed/17688660, retrieved on: 2018-07-04.
Gröber, U. (2011): Mikronährstoffe. Metabolic Tuning – Prävention – Therapie. 3. Aufl. Wissenschaftliche Verlagsgesellschaft mbH Stuttgart.
Gröber, U. (2007): Arzneimittel und Mikronährstoffe – Medikationsorientierte Supplementierung. 3. Aufl. Wissenschaftliche Verlagsgesellschaft Stuttgart.
Gröber, U. (2015): Interaktionen, Arzneimittel und Mikronährstoffe. 2. Aufl. Wissenschaftliche Verlagsgesellschaft Stuttgart.
Guan, F. et al. (2012): Deleterious effects of high concentrations of (-)-epigallocatechin-3-gallate and atorvastatin in mice with colon inflammation. Nutr Cancer. 2012; 64(6): 847-55. https://www.ncbi.nlm.nih.gov/pubmed/22716294, retrieved on: 2018-07-04.
Guandalini, S. (2011): Probiotics for prevention and treatment of diarrhea. J Clin Gastroenterol. 2011; 45 Suppl: S149-53. https://www.ncbi.nlm.nih.gov/pubmed/21992955, retrieved on: 2018-07-04.
Hering, N.A. und Schulzke, J.D. (2009): Therapeutic options to modulate barrier defects in inflammatory bowel disease. Dig Dis. 2009; 27: 450-54. https://www.karger.com/Article/Abstract/233283#, retrieved on: 2018-07-04.
Herold, G. (2017): Innere Medizin. Selbstverlag, Köln.
Higgins, J.A. und Brown, I.L. (2013): Resistant starch: a promising dietary agent for the prevention/treatment of inflammatory bowel disease and bowel cancer. Curr Opin Gastroenterol. 2013; 29(2): 190-94. https://www.ncbi.nlm.nih.gov/pubmed/23385525, retrieved on: 2018-07-04.
Internisten im Netz: Wann wird Durchfall gefährlich? Aktuelle Meldungen. https://www.internisten-im-netz.de/aktuelle-meldungen/aktuell/wann-wird-durchfall-gefaehrlich.html, retrieved on: 2018-07-04.
Jacobasch, G. und Dongowski, G. (2011): Ballaststoffe/Präbiotika: biologische Wirkungen und gesundheitsfördernde Effekte in der Prävention. In: Ebersdobler, H. und Meyer, A.: Praxishandbuch Functional Food. Behr’s Verlag.
Johnston, B.C. et al. (2006): Probiotics for pediatric antibiotic-associated diarrhea: a meta-analysis of randomized placebo-controlled trials. CMAJ. 2006; 175(4): 377-83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1534112/, retrieved on: 2018-07-04.
Kim, H. et al. (2005): Metabolic and pharmacological properties of rutin, a dietary quercetin glycoside, for treatment of inflammatory bowel disease. Pharm Res. 2005; 22(9): 1499-509. https://www.ncbi.nlm.nih.gov/pubmed/16132362, retrieved on: 2018-07-04.
Konturek, P.C. & Zopf, Y.Z (2017): Therapeutische Modulation der Darmmikrobiota beim Reizdarmsyndrom. Von Probiotika bis zur fäkalen Mikrobiota-Therapie. MMW-Fortschritte der Medizin 2017; 159 (S7): 1–5. https://www.ncbi.nlm.nih.gov/pubmed/18671775, retrieved on: 2018-07-04.
Kwon, K.H. et al. (2005): Dietary rutin, but not its aglycone quercetin, ameliorates dextran sulfate sodium-induced experimental colitis in mice: attenuation of pro-inflammatory gene expression. Biochem Pharmacol. 2005; 69(3): 395-406. https://www.ncbi.nlm.nih.gov/pubmed/15652231, retrieved on: 2018-07-04.
Lazzerini, M. & Wanzira, H. (2016): Oral zinc supplementation for treating diarrhea in children. Cochrane Database of Systematic Reviews 2016; Issue 12. Art No. CD005436. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD005436.pub5/pdf/abstract, retrieved on: 2018-07-04.
Mehmood, M.H. et al. (2015): Antidiarrhoeal, antisecretory and antispasmodic activities of Matricaria chamomilla are mediated predominantly through K+-channels activation. BMC Complement Altern Med. 2015; 15:75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4410481/, retrieved on: 2018-07-04.
Habtemariam, S. & Belai, A. (2018): Natural therapies of the inflammatory bowel disease: the case of rutin and its aglycone, quercetin. Min Rev Med Chem. 2018; 18(3): 234-43. https://www.ncbi.nlm.nih.gov/pubmed/28117024, retrieved on: 2018-07-04.
Mohammadi-Sartang, M. et al. (2017): Effects of supplementation with quercetin on plasma C-reactive protein concentrations: a systematic review and meta-analysis of randomized controlled trials. Eur J Clin Nutr. 2017; 71(9): 1033-39. https://www.ncbi.nlm.nih.gov/pubmed/28537580, retrieved on: 2018-07-04.
Nugent, A.P. (2005): Health properties of resistant starch. Nutrition Bulletin. 2005; 30: 27-54. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1467-3010.2005.00481.x, retrieved on: 2018-07-04.
Pari, L. (2008): Role of curcumin in health and disease. Arch Physiol Biochem. 2008; 114(2): 127-49. https://www.ncbi.nlm.nih.gov/pubmed/18484280, retrieved on: 2018-07-04.
Pernica, J.M. et al. (2017): Rapid enteric testing to permit targeted antimicrobial therapy, with and without Lactobacillus reuteri probiotics, for paediatric acute diarrhoeal disease in Botswana: A pilot, randomized, factorial, controlled trial. PLoS One. 2017: v12(10). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5633142/, retrieved on: 2018-07-04.
Pschyrembel Klinisches Wörterbuch (2014). 266. Aufl. De Gruyter Verlag Berlin.
Raghupahty, P. et al. (2006): Amylase-resistant starch as adjunct to oral rehydration therapy in children with diarrhea. J Pediatr Gastroenterol Nutr. 2006; 42(4): 362-8. https://www.ncbi.nlm.nih.gov/pubmed/16641573, retrieved on: 2018-07-04.
Ramakrishna, B.S. et al. (2008): A randomized controlled trial of glucose versus amylase resistant starch hypo-osmolar oral rehydration solution for adult acute dehydrating diarrhea. PLoS One. 2008; 3(2): e1587. https://www.ncbi.nlm.nih.gov/pubmed/18270575, retrieved on: 2018-07-04.
Ramakrishna, B.S. et al. (2000): Amylase-resistant starch plus oral rehydration solution for cholera. N Engl J Med. 2000; 342(5): 308-13. https://www.ncbi.nlm.nih.gov/pubmed/10655529, retrieved on: 2018-07-04.
Sazawal, S. et al. (2006): Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials. Lancet Infect Dis. 2006; 6(6): 374-82. https://www.ncbi.nlm.nih.gov/pubmed/16728323, retrieved on: 2018-07-04.
Sazawal, S. et al. (1995): Zinc supplementation in young children with acute diarrhea in India. N Engl J Med. 1995; 333(13): 839-44. https://www.ncbi.nlm.nih.gov/pubmed/7651474, retrieved on: 2018-07-04.
Sebai, H. et al. (2014): Antidiarrheal and antioxidant activities of chamomile (Matricaria recutita L.) decoction extract in rats. J Ethnopharmacol. 2014; 152(2): 327-32. https://www.ncbi.nlm.nih.gov/pubmed/24463157, retrieved on: 2018-07-04.
Sharma, R.A. et al. (2018): Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res. 2004 Oct 15;10(20):6847-54. https://www.ncbi.nlm.nih.gov/pubmed/15501961. retrieved on: 2018-07-04.
Steinmann, J. et al. (2013): Anti-infective properties of epigallocatechin-3-gallate (EGCG), a component of green tea. Br J Pharmacol. 2013; 168(5): 1059-73. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3594666/, retrieved on: 2018-07-04.
Topping, D.L. & Clifton, P.M. (2001): Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol Rev. 2001; 81(3): 1031-64. https://www.ncbi.nlm.nih.gov/pubmed/11427691, retrieved on: 2018-07-04.
Topping, D.L. et al. (2003): Resistant starch as a prebiotic and synbiotic: state of the art. Proc Nutr Soc. 2003; 62(1): 171-76. https://www.ncbi.nlm.nih.gov/pubmed/12749342, retrieved on: 2018-07-04.
Urbanska, M. et al. (2016): Systematic review with meta-analysis: Lactobacillus reuteri DSM 17938 for diarrhoeal diseases in children. Aliment Pharmacol Ther. 2016; 43(10): 1025-34. https://www.ncbi.nlm.nih.gov/pubmed/26991503, retrieved on: 2018-07-04.
World Health Organization (2005): The treatment of diarrhea: a manual for physicians and other senior health workers. 4. Auflage. http://apps.who.int/iris/bitstream/handle/10665/43209/9241593180.pdf;jsessionid=C2649E1DB9293C17AA0590850E7F3816?sequence=1, retrieved on: 2018-07-04.
Zeng, J. et al. (2008): Clinical trial: effect of active lactic acid bacteria on mucosal barrier function in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2008; 28(8): 994-1002. https://www.ncbi.nlm.nih.gov/pubmed/18671775, retrieved on: 2018-07-04.
Zhang, D.M. et al. (2017): A prospective control study of Saccharomyces boulardii in prevention of antibiotic-associated diarrhea in the older inpatients. Zhonghua Nei Ke Za Zhi. 2017; 56(6): 398-401. https://www.ncbi.nlm.nih.gov/pubmed/28592037, retrieved on: 2018-07-04.