Arthrosis is the wear and tear of the joint which is commonly the result of overstraining or incorrectly straining the joint over many years. Those affected suffer from pain and a limited range of movement. The disease cannot be cured. The goal of the treatment is to reduce joint-related symptoms and slow the progression of the disease. Vitamins and minerals help as a supplementary treatment with few side-effects. Find out here which nutrients can play a role in the treatment of arthrosis and how they can be correctly applied within the scope of micronutrient medicine.

Causes and Symptoms
What is arthrosis?
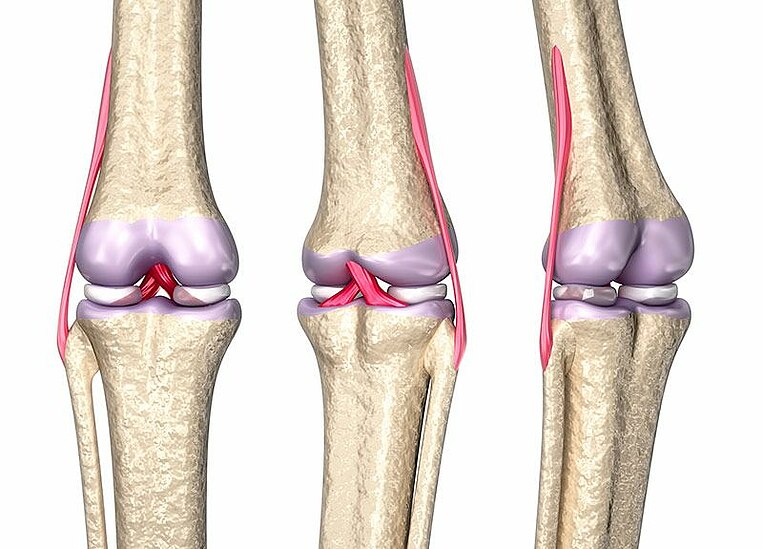
Arthrosis (arthrosis deformans) is one of the most common types of diseases affecting the joints. Arthrosis begins with a loss of cartilage. The process initially affects only the cartilage, but later spreads to the entire joint. Bone and cartilage begin to deteriorate and begin to lose stability and structure. This leads to a gradual loss of joint function and the development of painful inflammation (arthritis or joint inflammation). On top of this, detached bone fragments trigger inflammation in the joint mucous membranes. In the final stage, the bones begin to rub against each other and cause severe pain.
Arthrosis is a degenerative condition which progresses slowly. Inflammation (arthritis) initially appears for episodes which over time tend to become chronic.
In principal, arthrosis can affect any of the joints in the body. Knee joints (gonarthrosis), hip joints (coxarthrosis), and shoulder joints (omartrosis) are most commonly affected. But also jaw joints, wrist joints, arms, fingers (most commonly the thumb), toes, and small vertebrae in the spine can become affected.
Info
What is the difference between arthrosis, arthritis, rheumatism, and gout?
Arthrosis is the non-inflammatory deterioration of the joints and arthritis is joint inflammation. Arthritis can develop out of many types of disease, such as arthrosis, inflammation, or rheumatism. Uncontrollable inflammation of the joint is the cause of rheumatoid arthritis (rheumatism).
In contrast, gout is a metabolic disease caused by too much uric acid being present in the blood. This causes uric acid deposits to build up in the joints which causes extreme pain.
The causes of arthrosis
The causes (etiology) of arthrosis are varied and there may be several at the same one time. This means that in many cases it is not possible to identify one specific cause of the disease. Risk factors include:
- genetics
- age, menopause
- severe mechanical straining of the joint, for example, due to work or obesity
- incorrect joint position, injuries, and incorrect straining of the joint
- lack of physical activity
- Metabolic conditions, such as diabetes or high cholesterol levels
Identifying arthrosis
The deterioration of the cartilage is initially not noticeable, only later do problems develop. A typical symptom is pain after a period of inactivity, like in the first movements in the morning, which later subsides. Exertion of the affected joint is usually followed by pain (activity-related pain). In the later stages of the condition, pain while resting may develop.
Signs of acute infection are reddening, swelling, and thickening around the joint. Joint stiffness also affects joint function and mobility. A grinding sounds can be heard when moving the joint.
An advanced case of arthrosis can be identified in x-ray images by the narrowing of the joint space (space between the bones) and a malformation of the bone in the joint. For example, subchondral cysts may develop. These are cavities which develop when the bone beneath cartilage defects has completed deteriorated. They are filled with residual connective tissue and fluid.
Aim of the treatment
What is the standard treatment for arthrosis?
There is no cure for arthrosis, but it is often possible to stop or slow its progress. Common treatment methods are physiotherapy and sufficient light physical activity. If overweight, you should immediately try to lose weight. This relieves strain in the joints and reduces inflammation A diet that is low in fat but high in vitamins and dietary fibers is important.
Info
Too much inactivity starves the cartilage because it only receives nutrients for the cartilage cells from the joint fluid following movement.
Additionally, regular physical activity improves joint mobility due to the activation of muscles and ligaments.
Technical medical aids such as insoles, bandages, or joint supports (orthoses) are used to help relieve and stabilize the joints.
Medications
They are applied either as a cream directly to the skin or taken in tablet form. Additionally, doctors use corticosteroids (cortisone) which is injected directly into the joint.
If nothing else helps, and the pain is severe, doctors may prescribe opioids. There are weaker opioids, such as Codeine and Dihydrocodeine (for example DHC Plus®) or Tramadol (for example, Ultram®) - and strong types of opioids (morphine such as (Dolphine® or Avinza®).
Surgery
Surgery is seen as a treatment of last resort because it has certain risks - e.g., thrombosis or infection. The following surgical options are available:
- Arthroscopy with rinsing, shaving and debridement: In this procedure the specialist will rinse the joint with a saline solution (lavage). Some areas of cartilage or bone may also be smoothed out (shaving and debridement). Finally, the joint is again rinsed, which flushes out dead cartilage or bone fragments and inflammatory messenger substances. However, health insurance providers do not usually cover the cost of this procedure.
- Radiosynoviorthesis (RSO): In this procedure, a radioactive substance is injected into the joint which reduces the inflammatory activity in the joint membrane and therefore reduces pain levels.
- Artificial joint (Endoprothesis): The affected joint is replaced by an artificial joint. The most common procedures are replacement of the hip and knee joints.
- Arthrodesis: In this procedure, the ends of the bones are conjoined using screws which results in a complete stiffening of the joints. This procedure is only used in the most severe cases where the implantation of an artificial joint is no longer possible.
The aims of micronutrient medicine
As in the standard course of treatment, the aim of micronutrient medicine is to reduce pain and inflammation and improve joint mobility. The use of micronutrient supplements may reduce the need for medication, which often has side-effects. Also, the cartilage should have all necessary nutrients available to prevent further deterioration and to strengthen the remaining cartilage.
- Glucosamine, chondroitin, hyaluronic acid and collagen are all components of joint cartilage.
- Omega-3 fatty acids and the plant substances curcumin help reduce inflammation in the joints.
- Antioxidants help protect the cartilage.
- Calcium, vitamin D and vitamin K help strengthen the bones.
Treatment using micronutrients
Glucosamine and chondroitin help relieve the symptoms of arthrosis.
How they work:
Glucosamine and chondroitin sulfate are natural building blocks of the cartilage in the joints and provide the cartilage with nourishment. One of the aims of arthrosis treatment is stopping further deterioration of the cartilage. Glucosamine sulfate is anti-inflammatory and therefore reduces pain levels. This was confirmed during an extensive review (metastudy) which analyzed the findings of 80 studies carried out between 2003 and 2016.
A different metastudy compared the pain-reducing properties of glucosamine and chondroitin with those of standard pain medication The effects were overall weaker than the pain medication Celecoxib but not weaker than paracetamol. Another study showed that while Celecoxib was initially faster acting, after six months Celecoxib and Glucosamine/chondroitin were both equally as effective.
However, glucosamine and chondroitin sulfate are not equally effective in all patients:
Some patients were shown to have a slowing of the deterioration and a reduction of the pain levels; in others no effect was observed. Further research is required to determine the reasons for this.
Dosage and Recommended Use
Doctors tend to recommend taking a combination of glucosamine and chondroitin sulfate: 1500 to 2000 milligrams of glucosamine sulfate and 800 to 1200 milligrams of chondroitin sulfate per day taken at mealtimes.
Make sure the supplement contains glucosamine sulfate: Glucosamine is available as a sulfate or hydrochloride. According to the study results, sulfate is better. Its effects have been studied more and overall it appears to more effective than glucosamine hydrochloride. Glucosamine and chondroitin are often extracted from animal sources (crustaceans and animal cartilage). However, plant-based glucosamine is now available.
Due to the fact that our cartilage cells have very slow metabolisms, the supplements must be taken over a long period of time. Micronutritionists often recommend therapy intervals, for example, 8 to 10 weeks of supplement use followed by a 2 week pause.
Instructions if taking medication or during illness
It cannot be definitively ruled out that glucosamine has an influence on the blood sugar levels of diabetes patients or those with impaired sugar metabolism. Despite the fact that numerous studies have shown no negative effects, it is advisable to regularly monitor the blood sugar levels of diabetics who are taking a glucosamine supplement.
The chemical makeup of glucosamine and chondroitin is similar to that of certain types of blood-thinning medications and can increase the effects of these medications. These include coumarin derivatives, especially Warfarin (for example Coumadin®) The blood coagulation values (INR) should be regularly monitored when using coumarin derivatives and glucosamine/chondroitin supplements.
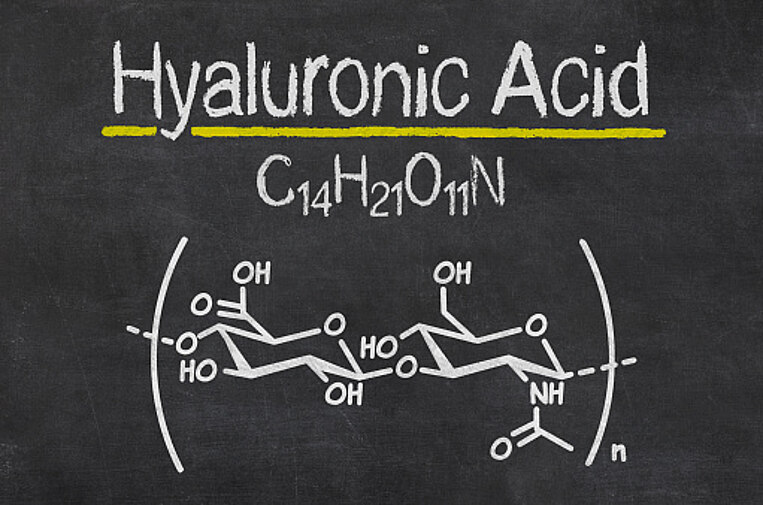
Hyaluronic acid lubricates the joints.
How it works:
Hyaluronic acid is often injected into the joints as part of the treatment of arthrosis. It is a component of the joint fluid and helps bind water. This enables hyaluronic acid to lubricate and protect the joint from friction and shocks.
It is not exactly known how hyaluronic acid works when taken as a supplement.
- Experiments carried out on human intestinal cells have shown that fragments of hyaluronic acid are more easily absorbed. A specially stained type of hyaluronic acid was identified in the joint fluid after being administered to animals.
- Scientists have also identified hyaluronic acid receptors in the intestinal tract. Docking with these receptors is suspected of triggering the release of anti-inflammatory substances which means hyaluronic acid can help reduce inflammation throughout the body.
Even though the exact way in which it works requires further study, numerous studies have shown that a dosage of between 48 and 240 milligrams of hyaluronic acid per day can reduce chronic knee pain compared to placebos.
Dosage and Recommended Use:
Micronutritionists recommend between 50 and 100 milligrams of hyaluronic acid per day to help relieve arthrosis-related pain. A continuous intake of hyaluronic acid is important as it is rapidly broken down by the body. Ideally, capsules, tablets, or powder should be consumed at mealtimes.
Hyaluronic acid can be extracted from chicken combs or through fermentation with microorganisms. The advantages of the production via fermentation is that the hyaluronic acid is suitable for vegans and vegetarians and is hypoallergenic.
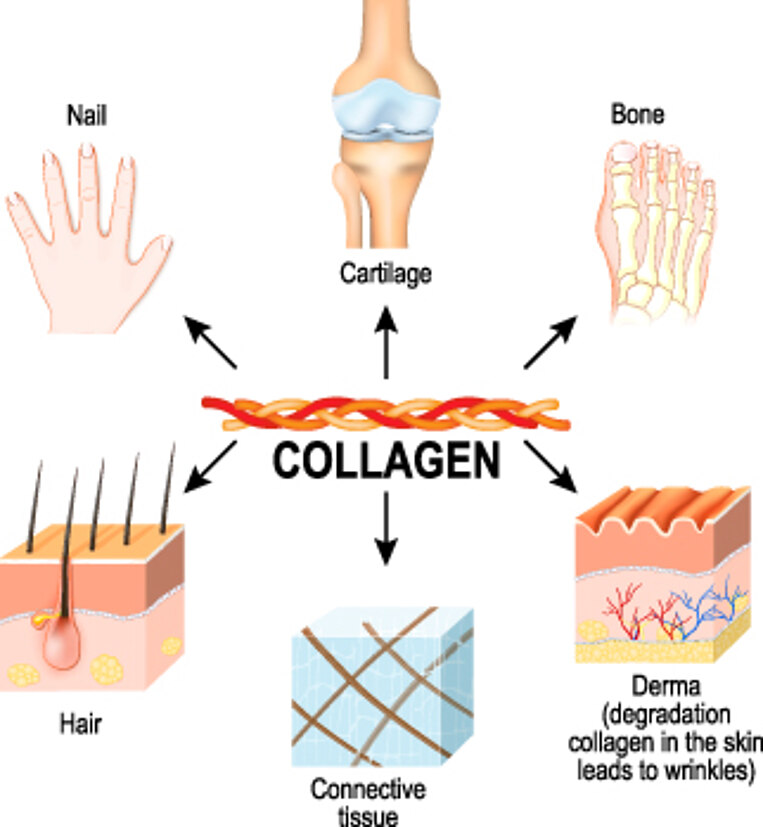
Chicken comb extract can contain proteins which can trigger an allergic reaction in those with chicken protein allergies.Collagen helps strengthen the cartilage while improving stability
How it works:
Collagen is a component of the joint cartilage and helps provide stability. There is a differentiation made between native collagen and collagen hydrolysate:
- Native collagen is collagen in its natural state. In contrast, denatured collagen has been destroyed by exposure to heat or acids. By having a regulating effect on the immune system, native collagen has anti-inflammatory properties.
- Collagen hydrolysate is collagen which has been broken down into small particles. This means it contains no fragments. Collagen hydrolysate nourishes the tissue and promotes regeneration of the cartilage.
Both of these types of collagen have been shown to be effective in the treatment of arthrosis:
Dosage and Recommended Use
Micronutritionists recommend a daily dosage of either 40 milligrams of native collagen or 5000 to 10,000 milligrams of collagen hydrolysate taken at mealtimes.
Make sure your purchased supplement contains native type 2 collagen. This is the type found in the cartilage, whereas the skin contains more of types 1 and 3. Type 2 has been successfully used in studies to treat joint problems.
Collagen and collagen hydrolysate are extracted from animal products and are not suitable for vegans or vegetarians. People with allergies should take care when choosing a collagen supplement made from animal products. It may be made from pig, chicken, cow, or fish products.Omega-3 fatty acids reduce joint inflammation.
How it works:
Arthrosis may be accompanied by inflammation of the membrane lining the joints (synovial membrane) which can in turn cause more damage to the cartilage. The body uses omega-3 fatty acids to produce anti-inflammatory messenger substances. This helps reduce inflammation in the joints. The most important omega-3 fatty acid in this case is eicosapentaenoic acid (EPA). It is a component of fish oil.
Patients who were found to have a high level of omega-3 in their blood showed less deterioration of the joint cartilage. Also, the use of fish oil for a period of eight weeks reduced knee joint pain and improved joint function when compared to the patients who were given a placebo. Omega-3 fatty acids in combination with glucosamine sulfate were found to be particularly effective.
Dosage and Recommended Use:
It is recommended to consume between 1000 and 2000 milligrams of omega-3 fatty acids per day with a high EPA level of between 400 and 800 milligrams. Omega-3 fatty acids should always be taken with a meal which contains fat. This enables them to be easily absorbed into the bloodstream.
You should pay special attention to the quality of the fish oil, and use only products with high levels of purity that are free from unwanted residual substances, such as heavy metals (like mercury) and pollutants
Info
Diet when suffering from arthrosis: It is not only important to take anti-inflammatory omega-3 fatty acids. Omega-6 fatty acids are equally as important. The body uses them to produce inflammation-promoting substances. As a result,the level of omega-6 fatty acids in your diet should be reduced. Omega-6 fatty acids are found in meat for example.
Determining your omega-3 levels: The omega-3 index
The omega-3 index is used to determine omega-3 levels in your blood. This test identifies the percentage of omega-3 fatty acids in the red cells. For patients with arthrosis, this test is recommended because low levels of omega-3 have been linked to more rapid progression of the disease.
On average, the omega-3 index is between five and eight percent. Ideally, it should be above eight percent.
Usage instruction when taking medications, before operations, and when suffering from certain types of diseases
Omega-3 fatty acids have blood-thinning properties and can increase the effects of blood-thinning medication starting at a dosage of 1000 milligrams. These include: Coumarin derivatives, such as (Marcumar®), acetylsalicylic acid (ASA, Aspirin®), Heparin (Clexane®) as well as new anticoagulants, such as Apixaban (Eliquis®), Dabigatran (Pradaxa®), Edoxaban (Lixiana®) and Rivaroxaban (Xarelto®). Talk to your doctor before taking omega-3 supplements.
Before any planned surgery and if suffering from blood coagulation disorders, you should discuss with your physician if you can use omega-3 supplements because of their blood-thinning properties.
In the event of the sudden development of liver disease, acute pancreatic, or gallbladder inflammation, then the use of omega-3 supplements should be stopped.
MSM: A provider of sulfur to the cartilaginous tissue
How it works
Methylsulfonylmethane is one of the body's most important sources of sulfur. Sulfur provides nutrients to the cartilage and is one of the fundamental building blocks of collagen and chondroitin sulfate.
MSM also reduces inflammation and neutralizes free radicals. Free radicals and oxidative stress damage the cartilage and result in further deterioration.
Micronutritionists recommend MSM for chronic pain patients. It is suspected that a substance produced during the metabolism of MSM blocks the pain signals from being transferred to the nerves. The analysis of several studies has shown that 3000 milligrams of MSM per day can slightly reduce arthrosis-related pain. How this directly effects the mobility and the daily life of those effected is not yet fully clear.
Dosage and Recommended Use:
For patients wanting to treat joint wear-and-tear, micronutritionists recommend between 1500 and 3000 milligrams of MSM per day. In combination with glucosamine and chondroitin sulfates, a daily MSM dosage of 500 milligrams is sufficient. Consuming MSM capsules at mealtimes improves their tolerability.
In rare cases, gastrointestinal problems, such as diarrhea, can develop. In this event, begin with a lower dosage (500 to 1000 milligrams) and then increase the dosage gradually.

Turmeric: Using plant substances to reduce pain levels
How it works
Turmeric, the "yellow spice", has anti-inflammatory properties. The active substance contained in the root is called curcumin and it inhibits the production of inflammation-promoting substances in the body and in turn reduces joint pain.
Curcumin also has antioxidant properties. It neutralizes free radicals, which can develop during inflammatory processes. Free radicals damage cells and can cause further deterioration of the cartilage.
An analysis of various studies, with a total of 800 participants suffering from knee arthrosis, confirmed that curcumin reduced knee pain level and improved quality of life when compared to the group of patients who were given a placebo. However, when compared to the pain medication ibuprofen, curcumin was less effective, although it was also free of side-effects.
Dosage and Recommended Use:
To reduce arthrosis-related pain levels, micronutritionists recommend up to 1000 milligrams of curcumin per day. Curcumin extract should be taken at mealtimes.
Generally, cucurmin is very poorly absorbed by the intestinal tract. However, there are options available to help improve the body's ability to absorb curcumin (increasing bioavailability). One available option is the use of piperine: This substance is extracted from pepper and prevents curcumin from being converted into ineffective substances by the liver and intestinal tract.
Instructions if taking medication or if suffering from gallstones
Unwanted interactions of curcumin with certain types of medications is possible. Curcumin can disrupt the function of the liver enzymes which are responsible for metabolizing medication. They may either reduce or increase the effects of the medication. If you are currently taking a dosage of medication, then discuss the use of curcumin supplements with your doctor.
Curcumin supplements should not be used if you are suffering from gallstones. Curcumin promotes the production of bile fluid. If a gallstone blocks the flow of bile fluid, this can result in biliary colic.
Antioxidants can help protect the cartilage.
How it works:
Too many free radicals in the body result in oxidative stress which can be harmful to cells. It is suspected that oxidative stress aids the progression of arthrosis. The body requires antioxidants to combat oxidative stress. The body can produce its own antioxidants (like enzymes) but they can also be consumed in our diet.
Vitamins A, C, and E are classified as antioxidants. Substances such as zinc, copper, or plant substances like curcumin, resveratrol and OPC can help neutralize harmful free radicals. A diet rich in antioxidants from fruit and vegetables is linked to a lower risk of cartilage damage.
Due to their beneficial properties, other types of antioxidants are recommended for the treatment of arthrosis:
- Vitamin C is required by the body for the production of collagen which helps with tissue stability, for example in the cartilage.
- Vitamin E helps relieve pain and reduces inflammation by inhibiting the production of inflammation-promoting substances. Studies have shown that taking high dosages of vitamin E can help improve arthrosis-related symptoms.
Study findings relating to the use of antioxidants in the treatment of arthrosis have been varied, with some reporting positive and others negative results. Future larger and more extensive studies will show to what extent antioxidants are able to help with treatment. An antioxidant-rich diet has shown to improve overall health, so it is worth trying it to see if it benefits arthrosis patients.
Dosage and Recommended Use:
Overall, if you are suffering from arthrosis, a diet rich in antioxidants from fruits and vegetables is recommended. Micronutritionists recommend a wide variety of antioxidant supplements - for example, 100 milligrams of vitamin C, up to 50 milligrams of vitamin E, and between 10 and 20 milligrams of zinc per day.
During vitamin E therapy a dosage of between 130 and 300 milligrams is recommended to treat the symptoms of arthrosis. In this case, a higher dosage of vitamin C is also recommended. When consuming 300 milligrams of vitamin E, the body should have access to 600 milligrams of vitamin C (ratio 1:2). For example, vitamin C is necessary for the body to allow vitamin E to regenerate itself after it has finished neutralizing free radicals.
Intake of high-dosage vitamin E supplements (more than 50 milligrams) should be discussed with a micronutritionist beforehand. Overdosing with vitamin E is possible.
What to look out for during vitamin E therapy or if taking medication
High-dosage vitamin E supplementation can have unwanted interactions with blood-thinning medications: The intake of both substances can cause a delay in coagulation of the blood. The affected types of medications include vitamin K antagonists (products containing Phenprocoumon, e.g., Marcoumar®, Marcumar
Calcium, vitamin D and K2 for arthrosis. Micronutrients for the bones
How it works:
Cartilage acts as a shock absorber and stops the bones from rubbing against one another. Deterioration of cartilage can lead to the bones becoming exposed and beginning to rub against each other. This causes damage to the end surfaces of the bones (e.g., subchondral cyst formation) and severe pain. This is why it is important to take bone nutrients, such as calcium, vitamin D, and vitamin K2 when suffering from arthrosis.
Calcium is the principal component of bones and ensures their stability.
Vitamin D regulates the absorption of calcium in the intestinal tract and helps supply the bones with the necessary calcium. Vitamin D also controls the maturation of bone cells. Vitamin D deficiency has been linked to the progression of cartilage deterioration and arthrosis. Researchers are also currently researching to determine whether vitamin D deficiency results in chronic pain. Initial studies have shown better joint function and pain level reduction as the result of vitamin D intake. Vitamin D most likely has a positive influence on the progression of the disease.
Vitamin K is required by the body to store calcium in the bones. It activates special bone proteins. Studies have shown that arthrosis patients with low vitamin K1 levels in their blood suffered from poorer function of the extremities (legs) and a higher risk of worsening joint deterioration. An initial study showed that taking vitamin K1 can slow this progression.
Dosage and Recommended Use:
Generally, between 1000 and 4000 international units per day of vitamin D are recommended. It is advisable to take a blood test to determine your vitamin D levels so any possible deficiency can be effectively treated. In the event of a severe deficiency, a high dosage may be necessary for a period of time.
For healthy bones, daily calcium intake should be at least 1000 milligrams. Vitamin K is advisable at a dosage of at least 100 micrograms.
Tips
Vitamin K in its K2 form (MK-7): There are various vitamin K subtypes. The MK7 form of vitamin K2 remains in the blood for longer than vitamin K1 and therefore has more time to be effective. As a result, K2 supplementation is recommended for the treatment of arthrosis.
A blood test to establish your vitamin D level
To be able to effectively treat a deficiency, it is necessary to first determine the levels of Vitamin D in the blood. The doctor will take a blood sample and send it to a laboratory where the levels of the circulating form of vitamin D (25(OH)-Vitamin D) will be determined. The ideal level in the blood is between 40 and 60 nanograms per milliliter.
Instructions if taking other medication or if suffering from kidney disease
Vitamin K should not be taken in combination with coumarin derivative blood-thinning medications (for example, Marcoumar®, Marcumar® and Falithrom®). It can inhibit the effects of the medication.
Thiazide diuretic medications reduce the amount of calcium being removed from the body by the kidneys. This means that the calcium remains in the blood. Because vitamin D also increases calcium levels in the blood, it should only be taken in combination with thiazide diuretics when the calcium levels are subject to regular monitoring. These include medications containing hydrochlorothiazide (Apo-Hydro®, Aquazide®).
Those with kidney diseases should discuss the use of calcium and vitamin D supplements with their doctor beforehand. Reduced kidney function can cause calcium to accumulate in the blood which in turn can cause vascular calcification. A doctor will carry out blood tests.
Dosage overview
Daily micronutrient recommended use in arthrosis | |
|---|---|
| Vitamins |
Vitamin D | 1000 to 4000 International Units (IU) |
Vitamin K (K2) | at least 100 micrograms (µg) |
Vitamin C | 100 milligrams (mg) (Higher during vitamin E therapy; ratio 2:1) |
Vitamin E | up to 50 milligrams (During vitamin E therapy up to 300 milligrams) |
Minerals | |
Calcium | at least 1000 milligrams |
Zinc | 10 to 20 milligrams |
Other nutrients | |
Glucosamine and chondroitin sulfates | 1500 to 2000 and 800 to 1200 milligrams |
Hyaluronic acid | 50 to 100 milligrams |
Collagen (Type 2) or Collagen hydrolysate | up to 40 milligrams or 5000 to 10,000 milligrams |
Omega-3 fatty acids | 1000 to 2000 milligrams containing 400 to 800 milligrams of EPA |
MSM | 500 to 3000 milligrams |
turmeric | up to 1000 milligrams |
Overview of recommended laboratory tests
Advisable blood tests when suffering from arthrosis | |
|---|---|
Normal reference range | |
Vitamin D | 40 and 60 nanograms per milliliter (ng/ml) |
Omega-3-Index | 5 to 8 percent, ideally above 8 percent |
Supporting the effects of medication with micronutrients
Non-steroidal antirheumatics: Reducing side-effects, supporting effectiveness
The use of non-steroidal antirheumatic medication (NSAR) can disrupt the body's ability to absorb and utilize certain types of vitamins. For example, the active pharmaceutical ingredient acetylsalicylic acid (ASA, Aspirin®) can reduce vitamin C levels in the gastric mucous membrane (lining of the stomach). Vitamin C is the most important antioxidant in the stomach and protects it against damage. The typical side-effects of acetylsalicylic acid are gastrointestinal complaints, such as stomach ache. Supplementation with vitamin C improves the stomach's tolerance to pain medication. To reduce damage to the lining of the stomach, micronutritionists recommend that you consume up to 1000 milligrams of vitamin C per day.
B vitamins improve the effects of non-steroidal antirheumatic medications - especially those with the active pharmaceutical ingredients Diclofenac, when both are injected directly into the affected area. Several studies have shown that Diclofenac in combination with B vitamins is more effective in relieving symptoms than Diclofenac alone. The studies did not focus solely on arthrosis, but also postoperative, bone fracture, and back pain levels.
To ensure Diclofenac (for example Voltaren®, Cataflam® and Zipsor®) is effective when taken in tablet form, you should ensure a sufficient intake of B vitamins - especially vitamin B1 (50 to 100 milligrams), vitamin B6 (50 to 100 milligrams), vitamin B12 (250 to 1000 micrograms) and folic acid (400 to 1000 micrograms). There are also study findings which suggest that B vitamins taken as capsules can also improve the effects of the medication.
Dosage overview
Daily micronutrient intake recommendations when using non-steroidal antirheumatics | |
|---|---|
Vitamin C | up to 1000 milligrams (mg) (when using acetylsalicylic acid ) |
Vitamin B1 | 50 to 100 milligrams (when using Diclofenac) |
Vitamin B6 | 50 to 100 milligrams (when using Diclofenac) |
Vitamin B12 | 250 to 1000 milligrams (µg) (when using Diclofenac) |
Folic Acid | 400 micrograms (when using Diclofenac) |
Summary
Arthrosis (joint wear and tear) is a disease which cannot be cured and is accompanied by joint pain and reduced range of movement. Cartilage and bone can be further damaged by overloading or incorrect straining of the joint. The goal of the treatment is to reduce the joint-related symptoms and slow the rate of cartilage deterioration.
Glucosamine and chondroitin sulfates are commonly the first-choice supplements in the treatment of arthrosis. They have been shown to reduce pain levels and inhibit inflammation. Their effects are amplified by the effect of omega-3 fatty acids: They intervene in the inflammatory process because the body uses them to produce anti-inflammatory messenger substances. Arthrosis is characterized by recurring inflammatory episodes triggered by small fragments of detached cartilage.
Hyaluronic acid acts as a lubricant for the joints: It helps bind water and protects against shocks. Collagen increases the stability of the cartilage, whereas sulfur (for example, MSM) is an important component of the makeup of the cartilage. Antioxidants such as vitamin C, vitamin E, or plant substances (e.g., curcumin and resveratrol) protect the cartilage, and defend against the harmful effects of free radicals. The body requires calcium, vitamin D, and vitamin K for strong bones.
Arthrosis patients often use pain medication. Especially when pain medications are used regularly over a long period of time, certain types can cause micronutrient deficiencies - for example, acetylsalicylic acid can cause vitamin C deficiency. B vitamins increase the effects of Diclofenac. The combination of the substances can cause a targeted increase in the effects.
Study and Source Index
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V. (AWMF) e.V. (AWMF) (2018): S2k-Leitlinie Gonarthrose. Homepage, http://www.awmf.org/uploads/tx_szleitlinien/033-004l_S2k_Gonarthrose_2018-01_1.pdf, retrieved on: 2018-06-05.
Baker, K.R. et al. (2012): Association of plasma n-6 and n-3 polyunsaturated fatty acids with synovitis in the knee: the MOST study. Osteoarthritis Cartilage. 2012 May;20(5):382-7. https://www.ncbi.nlm.nih.gov/pubmed/22353693, retrieved on: 2018-05-03.
Brien, S. et al. (2011): Meta-analysis of the related nutritional supplements dimethyl sulfoxide and methylsulfonylmethane in the treatment of osteoarthritis of the knee. Evid Based Complement Alternat Med. 2011; 2011:528403. https://www.ncbi.nlm.nih.gov/pubmed/19474240, retrieved on: 2018-05-03.
Brüggemann, G. et al. (1990): Results of a double-blind study of diclofenac + vitamin B1, B6, B12 versus diclofenac in patients with acute pain of the lumbar vertebrae. A multicenterstudy. Klin Wochenschr. 1990 Jan 19;68(2):116-20. https://www.ncbi.nlm.nih.gov/pubmed/2138684, retrieved on: 2018-05-16.
Bruyère, O. et al. (2012): Effect of collagen hydrolysate in articular pain: a 6-month randomized, double-blind, placebo controlled study. Complement Ther Med. 2012 Jun;20(3):124-30. https://www.ncbi.nlm.nih.gov/pubmed/22500661, retrieved on: 2018-05-03.
Bundesinstitut für Risikobewertung (BfR) (2010/2013): Glucosaminhaltige Nahrungsergänzungsmittel können ein Gesundheitsrisiko für Patienten darstellen, die Cumarin-Antikoagulantien als Blutgerinnungshemmer einnehmen. Stellungnahme Nr. 004/2010 des BfR vom 14. August 2009, ergänzt am 21. Januar 2013. http://www.bfr.bund.de/cm/343/glucosaminhaltige_nahrungsergaenzungsmittel.pdf, retrieved on: 2018-06-05.
Bundesinstitut für Risikobewertung (BfR) (2010/2013): Verwendung von Chondroitinsulfat in Nahrungsergänzungsmitteln. Stellungnahme Nr. 031/2007 des BfR vom 15. Juni 2007. http://www.bfr.bund.de/cm/343/verwendung_von_chondroitinsulfat_in_nahrungsergaenzungsmitteln.pdf, retrieved on: 2018-06-05.
Crowley, D.C. et al. (2009): Safety and efficacy of undenatured type II collagen in the treatment of osteoarthritis of the knee: a clinical trial. Int J Med Sci. 2009 Oct 9;6(6):312-21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2764342/, retrieved on: 2018-05-03.
Daily, J.W. et al. (2016): Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Med Food. 2016 Aug;19(8):717-29. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5003001/, retrieved on: 2018-05-15.
Dammann, H.G. et al. (2004): Effects of buffered and plain acetylsalicylic acid formulations with and without ascorbic acid on gastric mucosa in healthy subjects. Aliment Pharmacol Ther. 2004 Feb 1;19(3):367-74. https://www.ncbi.nlm.nih.gov/pubmed/14984384, retrieved on: 2018-05-16.
Debbi, E.M. et al. (2011): Efficacy of methylsulfonylmethane supplementation on osteoarthritis of the knee: a randomized controlled study. BMC Complement Altern Med. 2011 Jun 27; 11:50. https://www.ncbi.nlm.nih.gov/pubmed/21708034, retrieved on: 2018-05-03.
Deutsche Gesellschaft für Orthopädie und Orthopädische Chirurgie (DGOOC) (2018): S2k-Leitlinie Gonarthrose. http://www.awmf.org/uploads/tx_szleitlinien/033-004l_S2k_Gonarthrose_2018-01_1.pdf, retrieved on: 2018-05-02.
EFSA Panel on Dietetic Products, Nutrition and Allergies (2011): Statement on the safety of glucosamine for patients receiving coumarin anticoagulants. EFSA Journal 2011;9(12):2473. https://efsa.onlinelibrary.wiley.com/doi/epdf/10.2903/j.efsa.2011.2473, retrieved on: 2018-05-29.
Eiden, P. (2015): Prävention und Therapie der Arthrose – Raus aus dem Teufelskreis: Abnehmen und bewegen. Dtsch Arztebl 2015; 112(7): A-280 / B-242 / C-238. https://www.aerzteblatt.de/archiv/168060/Praevention-und-Therapie-der-Arthrose-Raus-aus-dem-Teufelskreis-Abnehmen-und-bewegen, retrieved on: 2018-05-02.
Gommans, Y.M.M. et al. (2017): The Effect of Prolonged Glucosamine Usage on HbA1c Levels and New-Onset Diabetes Mellitus in Overweight and Obese Middle-Aged Women. Am J Med. 2017 Jun;130(6):731-737.e6. https://www.ncbi.nlm.nih.gov/pubmed/28011309, retrieved on: 2018-05-29.
Gröber, U. (2011): Mikronährstoffe. Metabolic Tuning – Prävention – Therapie. 3. Aufl. Wissenschaftliche Verlagsgesellschaft mbH Stuttgart.
Gröber, U. (2014): Arzneimittel und Mikronährstoffe – Medikationsorientierte Supplementierung. 3. Aufl. Wissenschaftliche Verlagsgesellschaft mbH Stuttgart.
Gruenwald, J. et al. (2009): Effect of glucosamine sulfate with or without omega-3 fatty acids in patients with osteoarthritis. Adv Ther. 2009 Sep;26(9):858-71. https://www.ncbi.nlm.nih.gov/pubmed/19756416, retrieved on: 2018-05-03.
Haflah, N.H. et al. (2009): Palm vitamin E and glucosamine sulphate in the treatment of osteoarthritis of the knee. Saudi Med J. 2009 Nov;30(11):1432-8. https://www.ncbi.nlm.nih.gov/pubmed/19882056, retrieved on: 2018-05-16.
Helde-Frankling, M. et al. (2017): Vitamin D in Pain Management. Int J Mol Sci. 2017 Oct; 18(10): 2170. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5666851/, retrieved on: 2018-05-15.
Herold, G. et al. (2017): Innere Medizin 2017. 1. Aufl. Gerd Herold, Köln.
Hochberg, M.C. et al. (2016): Combined chondroitin sulfate and glucosamine for painful knee osteoarthritis: a multicentre, randomised, double-blind, non-inferiority trial versus celecoxib. Ann Rheum Dis. 2016 Jan;75(1):37-44. https://www.ncbi.nlm.nih.gov/pubmed/25589511, retrieved on: 2018-05-29.
Jensen, G.S. et al. (2015): Oral intake of a liquid high-molecular-weight hyaluronan associated with relief of chronic pain and reduced use of pain medication: results of a randomized, placebo-controlled double-blind pilot study. J Med Food. 2015 Jan;18(1):95-101. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4281855/, retrieved on: 2018-05-03.
Lubis, A.M.T. et al. (2017): Comparison of Glucosamine-Chondroitin Sulfate with and without Methylsulfonylmethane in Grade I-II Knee Osteoarthritis: A Double Blind Randomized Controlled Trial. Acta Med Indones. 2017 Apr;49(2):105-111. https://www.ncbi.nlm.nih.gov/pubmed/28790224, retrieved on: 2018-05-03.
Lugo, J.P. et al. (2016): Efficacy and tolerability of an undenatured type II collagen supplement in modulating knee osteoarthritis symptoms: a multicenter randomized, double-blind, placebo-controlled study. Nutr J. 2016 Jan 29;15:14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4731911/, retrieved on: 2018-05-03.
Mabey, T. et al. (2015): Role of Vitamin D in Osteoarthritis: Molecular, Cellular, and Clinical Perspectives. Int J Endocrinol. 2015: 383918. https://www.hindawi.com/journals/ije/2015/383918/, retrieved on: 2018-05-15.
Magaña-Villa, M.C. (2013): B-vitamin mixture improves the analgesic effect of diclofenac in patients with osteoarthritis: a double blind study. Drug Res (Stuttg). 2013 Jun;63(6):289-92. https://www.ncbi.nlm.nih.gov/pubmed/23526240, retrieved on: 2018-05-16.
Mibielli, M.A. et al. (2009): Diclofenac plus B vitamins versus diclofenac monotherapy in lumbago: the DOLOR study. Curr Med Res Opin. 2009 Nov;25(11):2589-99. https://www.ncbi.nlm.nih.gov/pubmed/19731994, retrieved on: 2018-05-16.
Oe, M. et al. (2016): Oral hyaluronan relieves knee pain: a review. Nutr J. 2016 Jan 27;15:11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4729158/, retrieved on: 2018-05-03.
Ogata, T. et al. (2018): Effects of glucosamine in patients with osteoarthritis of the knee: a systematic review and meta-analysis. Clin Rheumatol. 2018 Apr 30. https://www.ncbi.nlm.nih.gov/pubmed/29713967, retrieved on: 2018-05-29.
Onakpoya, I.J. et al. (2017): Effectiveness of curcuminoids in the treatment of knee osteoarthritis: a systematic review and meta-analysis of randomized clinical trials. Int J Rheum Dis. 2017 Apr;20(4):420-433. https://www.ncbi.nlm.nih.gov/pubmed/28470851, retrieved on: 2018-05-15.
Panahi, Y. et al. (2016): Mitigation of Systemic Oxidative Stress by Curcuminoids in Osteoarthritis: Results of a Randomized Controlled Trial. J Diet Suppl. 2016;13(2):209-20. https://www.ncbi.nlm.nih.gov/pubmed/25688638, retrieved on: 2018-05-15.
Peanpadungrat, P. (2015): Efficacy and Safety of Fish Oil in Treatment of Knee Osteoarthritis. J Med Assoc Thai. 2015 Apr;98 Suppl 3:S110-4. https://www.ncbi.nlm.nih.gov/pubmed/26387397, retrieved on: 2018-05-03.
Pohle, T. et al. (2001): Role of reactive oxygen metabolites in aspirin-induced gastric damage in humans: gastroprotection by vitamin C. Aliment Pharmacol Ther. 2001 May;15(5):677-87. https://www.ncbi.nlm.nih.gov/pubmed/11328262, retrieved on: 2018-05-16.
Ponce-Monter, H.A. et al. (2012): Effect of diclofenac with B vitamins on the treatment of acute pain originated by lower-limb fracture and surgery. Pain Res Treat. 2012;2012:104782. https://www.ncbi.nlm.nih.gov/pubmed/22135737, retrieved on: 2018-05-16.
Poulet, B. & Beier, F. (2016): Targeting oxidative stress to reduce osteoarthritis. Arthritis Res Ther. 2016 Jan 27;18:32. https://www.ncbi.nlm.nih.gov/pubmed/26818766, retrieved on: 2018-05-16.
Puigdellivol, J. et al. (2018): Effectiveness of a Dietary Supplement Containing Hydrolyzed Collagen, Chondroitin Sulfate, and Glucosamine in Pain Reduction and Functional Capacity in Osteoarthritis Patients. J Diet Suppl. 2018 Apr 27:1-11. https://www.ncbi.nlm.nih.gov/pubmed/29701488, retrieved on: 2018-05-03.
Sato, T. et al. (2012): Comparison of menaquinone-4 and menaquinone-7 bioavailability in healthy women. Nutr J. 2012 Nov 12;11:93. https://www.ncbi.nlm.nih.gov/pubmed/23140417, retrieved on: 2018-05-15.
Schett, G. et al. (2013): Diabetes is an independent predictor for severe osteoarthritis: results from a longitudinal cohortstudy. Diabetes Care. 2013 Feb;36(2):403-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3554306/, retrieved on: 2018-05-06.
Schulz, H.U. et al. (2004): Effects of acetylsalicylic acid on ascorbic acid concentrations in plasma, gastric mucosa, gastric juice and urine--a double-blind study in healthy subjects. Int J Clin Pharmacol Ther. 2004 Sep;42(9):481-7. https://www.ncbi.nlm.nih.gov/pubmed/15487806 , retrieved on: 2018-05-16.
Schurgers, L.J. et al. (2007): Vitamin K-containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7. Blood. 2007 Apr 15;109(8):3279-83. https://www.ncbi.nlm.nih.gov/pubmed/17158229, retrieved on: 2018-05-15.
Shea, M.K. et al. (2015): The association between vitamin K status and knee osteoarthritis features in older adults: the Health, Aging and Body Composition Study. Osteoarthritis Cartilage. 2015 Mar;23(3):370-8. https://www.ncbi.nlm.nih.gov/pubmed/25528106, retrieved on: 2018-05-14.
Shea, M.K. et al. (2017): Sufficient vitamin K status combined with sufficient vitamin D status is associated with better lower extremity function: a prospective analysis of two knee osteoarthritis cohorts. Arthritis Care Res (Hoboken). 2017 Oct 17. https://www.ncbi.nlm.nih.gov/pubmed/29045002, retrieved on: 2018-05-14.
Singh, J. et al. (1986): Piperine-mediated inhibition of glucuronidation activity in isolated epithelial cells of the guinea-pig small intestine: evidence that piperine lowers the endogeneous UDP-glucuronic acid content. J Pharmacol ExpTher. 1986 Feb;236(2):488-93. https://www.ncbi.nlm.nih.gov/pubmed/3080587, retrieved on: 2018-05-15.
Suantawee, T. et al. (2013): Oxidative stress, vitamin e, and antioxidant capacity in knee osteoarthritis. J Clin Diagn Res. 2013 Sep;7(9):1855-9. https://www.ncbi.nlm.nih.gov/pubmed/24179881, retrieved on: 2018-05-16.
Tantavisut, S. et al. (2017): Effect of vitamin E on oxidative stress level in blood, synovial fluid, and synovial tissue in severe knee osteoarthritis: a randomized controlled study. BMC Musculoskelet Disord. 2017 Jun 29;18(1):281. https://www.ncbi.nlm.nih.gov/pubmed/28662656, retrieved on: 2018-05-16.
Thomas. S. et al. (2018): What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology (Oxford). 2018 May 1;57(suppl_4):iv61-iv74. https://www.ncbi.nlm.nih.gov/pubmed/29684218, retrieved on: 2018-05-06.
U.S. National Library of Medicine (2017): Glucosamine Sulfate. https://medlineplus.gov/druginfo/natural/807.html, retrieved on: 2018-05-29.
Usha, P.R. et al. (2004): Randomised, Double-Blind, Parallel, Placebo-Controlled Study of Oral Glucosamine, Methylsulfonylmethane and their Combination in Osteoarthritis. Clin Drug Investig. 2004;24(6):353-63. https://www.ncbi.nlm.nih.gov/pubmed/17516722, retrieved on: 2018-05-03.
Van Vijven, J.P. et al. (2012): Symptomatic and chondroprotective treatment with collagen derivatives in osteoarthritis: a systematic review. Osteoarthritis Cartilage. 2012 Aug;20(8):809-21. https://www.ncbi.nlm.nih.gov/pubmed/22521757, retrieved on: 2018-05-03.
Wang, Y. et al. (2016): Association Between Dietary Intake of Antioxidants and Prevalence of Femoral Head Cartilage Defects and Bone Marrow Lesions in Community-based Adults. J Rheumatol. 2016 Oct;43(10):1885-1890. https://www.ncbi.nlm.nih.gov/pubmed/27481903, retrieved on: 2018-05-16.
Wangroongsub, Y. et al. (2010): Comparable clinical outcomes between glucosamine sulfate-potassium chloride and glucosamine sulfate sodium chloride in patients with mild and moderate knee osteoarthritis: a randomized, double-blind study. J Med Assoc Thai. 2010 Jul;93(7):805-11. https://www.ncbi.nlm.nih.gov/pubmed/20649060, retrieved on: 2018-05-29.
Yong, W.C. et al. (2017): Effect of vitamin D supplementation in chronic widespread pain: a systematic review and meta-analysis. Clin Rheumatol. 2017 Dec;36(12):2825-2833. https://www.ncbi.nlm.nih.gov/pubmed/28812209, retrieved on: 2018-05-15.
Zeng, C. et al. (2015): Effectiveness and safety of Glucosamine, chondroitin, the two in combination, or celecoxib in the treatment of osteoarthritis of the knee. Sci Rep. 2015 Nov 18;5:16827. https://www.ncbi.nlm.nih.gov/pubmed/26576862, retrieved on: 2018-05-29.
Zhu, X. et al. (2018): Comparative effectiveness of glucosamine, chondroitin, acetaminophen or celecoxib for the treatment of knee and/or hip osteoarthritis: a network meta-analysis. Clin Exp Rheumatol. 2018 Jan 31. https://www.ncbi.nlm.nih.gov/pubmed/29465368, retrieved on: 2018-05-29.