High blood pressure (hypertension) causes damage to the blood vessels which in the long term leads to calcification of the arteries. Certain types of micronutrients, such as magnesium, potassium, and vitamin D regulate and help reduce blood pressure levels. This often means that the dosage of blood pressure lowering medications can be reduced and also reduces the risk of further damage to the blood vessels. Find out all you need to know about micronutrient medicine and blood pressure here.

Causes and Symptoms
Blood pressure is the pressure that the blood applies to the blood vessels. When the blood pressure levels are too high this is known as hypertension. There are many possible causes: being overweight, alcohol, smoking, stress and lack of physical exercise. High blood pressure can also develop during pregnancy .
There are two values which determine blood pressure: The systolic and the diastolic value. A healthy blood pressure is 120 over 80 millimeters of mercury (mmHg).
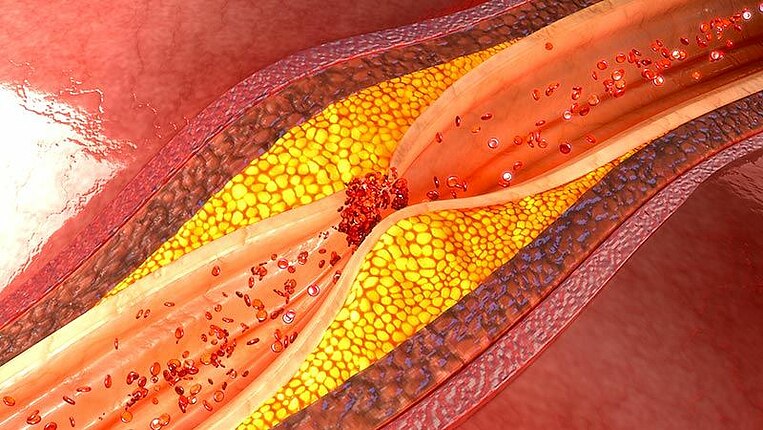
There are few outwardly visible symptoms. Symptoms such as headaches, vertigo (dizziness) and restlessness are possible. High blood pressure often goes undiscovered, and this is exactly what makes it so dangerous. Especially when other risk factors, such as high cholesterol and diabetes are present, the vascular system can suffer damage. The results are arteriosclerosis, stroke, or heart disease, such as coronary heart disease and heart failure. In the long-term, high blood pressure damages the kidneys, eyes, and even the brain.
Aim of the treatment
What is the standard treatment for high blood pressure?
The aim is to achieve a permanent normalization of the blood pressure levels. Doctors urgently recommend a change in lifestyle. If overweight, weight loss is advisable but you should also abstain from smoking and consuming alcohol. Regular physical exercise is also beneficial. If these measures do not lead to a sufficient reduction in blood pressure levels, your doctor will prescribe medication:
Diuretic medication increases the amount of excess water expelled through the kidneys. This causes a reduction of the blood fluid levels and blood pressure begins to fall. A type of medication for the treatment of high blood pressure is hydrochlorothiazide (HCT), for example Disalunil®.
Betablockers act by blocking the cardiac docking receptors for blood pressure-increasing chemical messenger substance, for example, stress hormones. You can recognize betablockers by the fact that the active pharmaceutical ingredient name ends in "olol", for example Bisoprolol (Concor®) and Metoprolol (Beloc®).
ACE inhibitors stop the production of the high pressure-causing hormone angiotensin II. This hormone is normally responsible for keeping the blood vessels narrow and increasing the pressure in the blood vessels. This type of blood pressure medication includes Ramipril (Altace®), Captopril (Capoten®) or Enalapril (Vasotec®). All these active pharmaceutical ingredients end with "pril".
Angiotensin receptor blockers act by blocking the cardiac docking receptors for the blood pressure-increasing hormone angiotensin II. These are known as sartans. They are recognizable by the fact that all the active pharmaceutical ingredient names end in "sartan", for example, Candesartan (Candecor®), Losartan (Lorzaar®) or Valsartan (Diovan®).
Calcium antagonists dilate the blood vessel to ensure that there is more room for the blood to pass through which lowers blood pressure. Examples of active pharmaceutical ingredients in calcium antagonists are Amlodipine (Norvasc®), Nimodipine (Nimotop®) and Verapamil (Isoptin®).
The aims of micronutrient medicine
Micronutrients can naturally reduce blood pressure levels. A healthy and balanced diet is important to achieve this. Vitamins and minerals promote the dilation of the blood vessels and improve the flow properties of the blood. This delays the start of treatment with blood-lowering medication or even makes medication unnecessary.
The correct administration of certain types of micronutrients can also reduce the risk of secondary diseases. Antioxidants protect the blood vessels from further damage. Micronutritionists normally recommend a multisupplement product which contains several different types of antioxidants.
Treatment using micronutrients
Magnesium to treat high blood pressure
How it works
Magnesium regulates muscular tension in the body. It helps the vascular musculature to relax and improves the elasticity of the blood vessels. This has a direct effect on blood pressure levels.
The findings of a metastudy showed that a magnesium intake increase of 100 milligrams per day reduced the risk of high blood pressure by 5 percent. The metastudy reviewed the findings from several high-quality medical studies to obtain accurate results.
Magnesium is also proven to reduce pre-existing high blood pressure levels.
Dosage and Recommended Use:
The response rate to magnesium can vary greatly from patient to patient: On average, 400 milligrams of magnesium per day will reduce the systolic value by up to 4 millimeters of mercury and the diastolic value by up to 3 millimeters of mercury. In a different study, 370 milligrams of magnesium led to only a minimal drop in blood pressure levels.
The recommended dosage for someone with healthy blood pressure levels is between 400 and 700 milligrams per day. Ideally, before beginning high-dosage supplementation with magnesium (more than 300 milligrams per day), a doctor should be consulted.
Tips
Magnesium is available in combination with taurine; this is known as magnesium taurate. Taurine regulates the heartbeat and has blood-pressure lowering properties.
Laboratory Tests
If suffering from high blood pressure, a blood test to determine the magnesium levels is advisable. Magnesium is mainly contained within the cells: Red blood cells contain three times more magnesium than the blood liquid (serum). Therefore, it is better when your doctor tests for the magnesium levels in whole blood - which contains the red blood cells.
Expert Knowledge
The normal magnesium levels in whole blood is between 1.38 and 1.50 millimoles per liter (mmol/l).
Magnesium: Instructions if taking medication or if suffering from disease
Magnesium can affect certain types of medication by binding with them and making them ineffective. These include antibiotics (especially gyrase inhibitors and tetracycline) and osteoporosis medication (bisphosphonates):
- Gyrase inhibitors Ciprofloxacin (e.g.Ciloxan®, Ciprobay®), Enoxacin (e.g., Enoxor®), Levofloxacin (e.g., Tavanic®), Moxifloxacin (e.g., Avalox®), Norfloxacin (e.g., Bactracid®, Norfluxx®) and Ofloxacin (e.g., Floxal®, Tarivid®)
- Tetracycline: Tetracycline (e.g., Achromycin®, Supramycin®, Tefilin®), Doxycycline (e.g., Supracyclin®, Vibramycin®), Minocycline (e.g., Aknosan®, Skinocyclin®)
- Bisphosphonates: Alendronate (e.g., Fosamax®, Tevanate®), Clodronate (e.g.Bonefos®), Etidronate (e.g., Didronel®), Ibandronate (Bondronat®), Pamidronate (Aredia®), Risedronate (Actonel®) and Tiludronate (Skelid®)
If using any of these medications, then a break of at least two hours should be observed between taking the medication and using a magnesium supplement.
Those with chronic kidneys disease use supplements to increase their magnesium intake. Weakened kidneys are not able to effectively excrete excess magnesium. The supplemented magnesium would begin to accumulate in the blood.
Taurine for a healthy heartbeat
How it works
Taurine is a by-product of the breaking down of amino acids which are produced in the metabolism and enter the body with food. Studies on cells and animals have shown that taurine promotes the strength of the heartbeat and also keeps the heart rhythm in balance.
Researchers attribute taurine with blood pressure-lowering properties: In a study using placebos, a daily dosage of 1600 milligrams of taurine reduced blood pressure levels on average by 7.2 (systolic value) and 4.7 millimeters of mercury (diastolic value). Using placebos in a study provides a good indication as to the effectiveness of a medication. However, the study was small with only 120 participants. Larger studies are due to be carried out in the future.
Dosage and Recommended Use:
To reduce blood pressure levels, micronutritionists recommend between 1500 and 4000 milligrams of taurine per day, often in combination with magnesium. This complete dosage should be spread throughout the day.
In rare cases, a dosage of over 2000 milligrams can cause stomach problems, such as nausea, diarrhea, and fatigue. Further problems tend to develop when taurine is consumed in the form of energy drinks, which usually also contain caffeine. These can cause increases in pulse and blood pressure. This is most probably linked to the caffeine which has stimulant effects. Taurine intake via energy drinks is not recommended as a blood pressure treatment.
Taurine: Care are should be taken during pregnancy, when breastfeeding, and when sick.
There is currently an insufficient amount of information available about the effects of taurine during pregnancy and when breastfeeding. Therefore, women who are pregnant or breastfeeding should avoid using taurine supplements.
The regulation of taurine levels in the blood is disrupted in those patients with kidney disease. Normally, taurine is removed from the body via the kidneys. Therefore, your doctor should critically assess the benefits of taurine supplements if you are suffering from reduced kidney function.
Taurine may also lower blood sugar levels. This has been shown in studies with animals. Therefore, diabetics who wish to use taurine supplements should check their blood sugar level more regularly. In the event that low blood sugar levels are confirmed, the dosage of either the diabetes medication or the taurine supplement can be adjusted accordingly.
Those with epilepsy who wish to use taurine supplements should consult a doctor beforehand. In studies with animals, taurine was found to have seizure-relieving as well as seizure-increasing properties. The seizure-increasing effects are possibly caused by the blood sugar-reducing (hypoglycemic) effects of taurine. Similar effects have not been observed in humans, with the exception of when taurine was consumed via energy drinks. High-level consumption of energy drinks triggered seizures in those with epilepsy. It is unclear if this was solely due to the taurine or the combination with caffeine and/or alcohol.
Omega-3 fatty acids allow the blood to flow better
How it works
Omega-3 fatty acids promote the dilation of the blood vessels and therefore reduce blood pressure levels. Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are especially important. A high-quality metastudy which reviewed more than 70 individual studies showed: Fatty acids such as EPA and DHA reduce systolic blood pressure by an average of 4.51 and the diastolic blood pressure by 3.05 millimeters of mercury (mmHg). Although, researchers cannot agree if fatty acids are equally as effective for all high blood pressure patients.
Omega-3 fatty acids also reduce the risk of developing secondary diseases. They slow the rate of the build-up of deposits in the blood vessels while having a stabilizing effect. If you have a high level of health-promoting fatty acids in the blood (an omega-3 index of at least 8 percent) then the probability of dying due to a heart attack is 30 percent lower.
Dosage and Recommended Use:
The American Heart Association recommends at least two portions of oily fish per week. If this is not possible, then doctors recommend taking omega-3 supplements. 1500 and 2500 milligrams with the highest available percentage of EPA is advisable per day.
All fatty acids supplements should be taken with food.
They are better absorbed into the bloodstream via the intestine when consumed with fat contained in the meal.
Tips
Ensure that fish oil products are high quality. High quality products are subjected to cleansing processes to remove pollutants and other unwanted residues.
Blood tests: The omega-3 index.
The omega-3 index confirms how good the intake of omega-3 fatty acid is. This test is advisable for those with cardiovascular diseases. The test identifies the amount of omega-3 fatty acids contained in the red blood cells and calculates the findings as a percentage.
Expert Knowledge
If the percentage is above 8 percent then the intake of omega-3 is very good. An index of below 4 percent confirms an insufficient intake of omega-3.
Omega-3 Fatty Acids: Instructions when using blood-thinning medication, during illness, and before operations:
Omega-3 fatty acids have blood-thinning properties and can increase the effects of blood-thinning medication starting at a dosage of 1000 milligrams. Talk to your doctor before using omega-3 supplements: If deemed necessary, a doctor can carry out a prothrombin time (PT Quick) test and carry out any adjustment to the medication dosage.
Examples are blood-thinners include coumarin derivatives (e.g., Marcumar®), Warfarin (Coumadin®), acetylsalicylic acid (ASA, Aspirin®), Heparin (Clexane®) as well as new anticoagulants, such as Apixaban (Eliquis®), Dabigatran (Pradaxa®), Edoxaban (Lixiana®) and Rivaroxaban (Xarelto®).
In the event that liver disease, acute pancreatic or gallbladder inflammation suddenly develop, stop taking omega-3 supplements. If you have a blood coagulation disorder, please discuss the use of omega-3 supplements with your doctor beforehand.
If surgery is planned, talk to your doctor to find out if it is necessary to stop taking omega-3 supplements.
Vitamin D deficiency increases the risk of high blood pressure
How it works
Vitamin D inhibits the production of the blood pressure hormone renin which contributes to high blood pressure levels. Vitamin D also influences the metabolism of calcium in the vascular cells: It reduces the muscle relaxant properties of calcium and is therefore indirectly involved in the dilation of the blood vessels.
A vitamin D insufficiency can increase the risk of high blood pressure by 300% for women and 600% for men. This was observed in two major observational studies. Whether vitamin D reduces blood pressure levels in all those affected is currently being studied: Initial medical studies show positive effects in cases were the patient had a pre-existing vitamin D deficiency.
Dosage and Recommended Use:
The vitamin D dosage is based on the vitamin D levels in the blood. Find out more about the correct dosage here. If the vitamin D level is not known, between 2000 and 4000 international units (IU) per day are recommended to counteract an increase in blood pressure.
Vitamin D is a fat-soluble vitamin. This means that it can only be correctly absorbed by the intestinal wall when consumed with fat. Always take vitamin D supplements at meal times.
Identifying a vitamin D deficiency
Because high blood pressure patients are often found to have a vitamin D deficiency, it is advisable to undergo blood testing to determine vitamin D blood levels. The laboratory blood test will determine the level of the vitamin D type which circulates in the bloodstream - 25-hydroxy vitamin D.
Expert Knowledge
The optimal vitamin D value is between 40 and 60 nanograms per milliliter (ng/ml) or between 100 and 150 nanomoles per liter (nmol/l).
Vitamin D: Instructions if taking medications or during illness
Those with kidney disease should avoid taking vitamin D before consulting their doctor first. Kidney patients have problems with the mineral balance in their body. They may have too high calcium levels. Because vitamin D promotes the absorption of calcium in the intestinal tract, calcium levels in the blood can increase sharply. Also, patients with kidney stones (which contain calcium) must be careful.
Patients with the inflammatory connective tissue disease sarcoidosis (also known as Boeck's disease) should not supplement with vitamin D: Patients with sarcoidosis often have high calcium levels in their blood, which may increase further if using vitamin D supplements.
Thiazide diuretic medications, containing the active substances hydrochlorothiazide (Esidrix®), xipamide (Aquaphor®) and indapamide (Natrilix®), reduce the levels of calcium removed from the body by the kidneys. This leads to increased levels of calcium in the blood. Because vitamin D also increases the calcium levels in the blood, vitamins D should only be taken in combination with thiazide diuretics when the calcium level is subject to regular monitoring.
Arginine improves vascular function
How it works
The amino acid arginine is the chemical precursor of the chemical messenger substance nitric oxide (NO). Nitric oxide dilated the blood vessels to ensure that there is more room for the blood.
An analysis of various metastudy findings showed: For high blood pressure patients, arginine can reduce the systolic value by between 2.2 and 5.4 millimeters of mercury and the diastolic value by between 2.7 and 3.1 millimeters of mercury.
Dosage and Recommended Use
Micronutritionists recommend taking between 2000 and 6000 milligrams of arginine per day. The intake of arginine should be spread throughout the day and ideally between meals: This allows arginine to be optimally absorbed by the intestinal tract.
A dosage above 6000 to 9000 milligrams of arginine per day can cause gastrointestinal problems, such as diarrhea and nausea.
A blood test to determine arginine levels
For patients with high blood pressure levels, a blood test to allow the doctor to determine the arginine levels in your blood is advisable. There is also an ADMA test. ADMA (asymmetric dimethylarginine) is a substance produced in the body which inhibits the production of nitric oxide, the blood vessel-dilating chemical messenger substance from arginine. High ADMA levels are associated with high blood pressure levels and other types of cardiovascular disease. The desired balance between ADMA and arginine can be achieved by taking arginine supplements.
Expert Knowledge
Plasma values of below 100 micromoles per liter (µmol/l) is defined as a deficiency. According to medical studies, arginine levels of between 100 and 300 micromoles per liter lead to a relaxation of the blood vessel caused by the chemical messenger substance nitric oxide (NO). The ideal ADAM/arginine ratio is between 50:1 and 100:1.
Arginine: What to watch out for during pregnancy, when breastfeeding, when taking medications, and while ill.
There is currently an insufficient level of study literature available on the use of arginine during pregnancy. Initial studies have shown beneficial effects of arginine in the prevention of pre-eclampsia (pregnancy poisoning). However, use of arginine supplements by pregnant women without monitoring by a doctor is not recommended.
The herpes group of viruses require arginine to reproduce. Arginine supplements should not be used by patients who suffer from recurring herpes outbreaks. It can re-activate dormant viruses and trigger infection.
If you are currently taking medication which has blood vessel-dilating effects similar to those of arginine – stimulation of the release of nitric oxide nitrovasodilator) - then consult your doctor beforehand. A dosage adjustment may be necessary. These include the nitrates (Mono Mack®, Ismo®), Molsidomin (Corvaton®, Molsibeta®) and Nitroprusside (Nipruss®).
The erectile dysfunction medication Sildenafil (Viagra®) should not be taken with arginine.
Potassium deficiency causes hypertension
How it works
Potassium is involved in the regulation of blood pressure levels. A deficiency leads to an increase in blood pressure levels. Additionally, patients with high blood pressure require more potassium than healthy individuals.
Several studies have shown potassium reducing previously high blood pressure levels: An overall intake of between 3500 and 4600 milligrams per day reduced the systolic value in adults by around 3.49 and the diastolic value by 1.96 millimiters of mercury.
Dosage and Recommended Use:
micronutritionists recommend between 2000 and 3000 milligrams per day depending on the blood potassium levels. Take smaller doses of potassium throughout the day. The individual potassium dose should not exceed 500 milligrams. Taking the supplement at mealtimes makes it more tolerable for the stomach.
Talk to your doctor before beginning to use potassium supplements. If you are not suffering from a deficiency you may develop excessive levels of potassium. This can lead to cardiac arrhythmia.
Test your potassium levels
Patients with high blood pressure should have their potassium levels checked to rule out a possible deficiency. The normal reference value range for potassium is between 3.6 and 4.8 millimoles per liter of blood serum (mmol/l).
Potassium: Care should be taken if suffering from kidney problems and if using blood pressure and diuretic medication
Potassium is expelled from the body via the kidneys. If the kidneys are not working correctly then potassium can begin to collect in the body. Depending on the severity of the kidney problems, potassium intake levels should not exceed between 1500 to 2000 milligrams per day. Patients with kidney problems should only use potassium supplements after consulting their doctor.
Blood pressure lowering medication, such as Rampiril (e.g., RamiLich®) and Lisinopril (e.g., LisiLich®) can reduce the amount of potassium being expelled from the body by the kidneys. An excessive level of potassium may develop with the use of potassium supplements. The same applies to AT-1 blocker, with the active pharmaceutical ingredients Amlodipine (Norvasc®) and Candesartan (e.g., Atacand® or Blopresid®). Patients who are using blood pressure-lowering medication should use potassium supplements.
Even if using cardiac glycosides (Digacin® oder Lanicor®) or potassium sparing diuretics (Diaphal®, Diursan®), you should avoid using potassium supplements. Potassium can reduce the effectiveness of cardiac glycosides. The use of potassium-sparing diuretics increases the risk of hyperkalemia (excessive levels of potassium).
Is an intestinal flora imbalance related to high blood pressure? How probiotics can help
How it works
In the last few years, scientists have discovered new correlations between intestinal health and various diseases, including heart and metabolic conditions. An intestinal flora imbalance may be related to high blood pressure.
Beneficial bacteria (probiotics) are able to help normalize intestinal flora imbalances: They displace harmful bacteria from the intestinal tract. However, the exact mechanism which help them reduce blood pressure is still not fully understood.
Expert Knowledge
It has been shown that probiotics create bioactive protein components which inhibit the angiotensin converting enzyme. They most likely act as the body's own ACE inhibitor. There is also evidence that short-chain fatty acids created during fermentation can also help to regulate blood pressure levels.
Probiotics were shown to reduce the systolic value by 3.56 and the diastolic value by 2.38 millimeters of mercury on average. The decrease was most notable in study participants who had the highest baseline blood pressure levels (above 135/85 millimeters of mercury). This was demonstrated in the first metastudy analyzing the findings of nine studies with more than 500 participants.
Dosage and Recommended Use:
Studies report that at least 1 billion (109) bacteria per day are necessary, and the more the better: The greatest effect was observed following the intake of 100 billion (1011) bacteria.
Doctors recommend multi-species supplements with various types of bifdobacteria and lactobacilli: The reduction was found to be greater when various types of bacteria were used and not only one individual type.
Info
Together, the survival chances of the beneficial bacteria in the intestinal tract are greater (teamwork). They are able to better withstand the passage through the intestines and colonize the tract. Also, different types of bacteria produce different types of metabolic products which in turn may be useful to other bacteria.
Probiotics: Instructions if suffering from illness.
There is a possibility that some types of probiotics may produce histamine in the intestinal tract. These include: Lactobacillus casei, Lactobacillus delbrueckii ssp. bulgaricus, Lactobacillus reuteri, Lactococcus lactis and Enterococcus faecium. This means that probiotic supplements may cause problems for patients with histamine intolerance.
Very weak patients with suppressed immune systems, those with a central venous catheter, (e.g., during chemotherapy), heart valve disease or with short bowel syndrome should not use probiotics.
Antioxidants: The radical scavengers in the blood vessel.
How they work
Antioxidants catch free radicals and can protect the blood vessels from further damage.
For instance, vitamin A, vitamin E and vitamin C or the minerals selenium and zinc are important. Coenzyme Q10 also belongs to the antioxidants.
Coenzyme Q10 and vitamin C can also help in the reduction of blood pressure levels: Vitamin C increases the availability of the blood vessel-dilating chemical messenger nitric oxide, while coenzyme Q10 promotes the production of the chemical messenger.
Dosage and Recommended Use:
Micronutritionists usually recommend a broad range of different antioxidants. These will target various regions in the body and are needed to help regenerate themselves after they have neutralized free radicals. Study showed that 500 milligrams of vitamin C and 200 milligrams of coenzyme Q10 were effective in reducing blood pressure levels.
Antioxidants are best absorbed in the intestinal tract when consumed at mealtimes.
Coenzyme Q10 and Vitamin C: What to watch out for when suffering from an illness or taking medication
Coenzyme Q10 can reduce the effectiveness of certain types of blood-thinning medications. These include Cumarine, containing the active substances phenprocoumon (e.g., Marcumar®, Falithrom® and Marcuphen®) and Warfarin (Coumadin®). These effects have been reported when using coenzyme Q10 dosages as low as between 30 and 100 milligrams. Consult your doctor before using coenzyme Q10 supplements. A doctor uses the PT quick test (PT: prothrombin time) to determine if coenzyme Q10 supplements can be used.
Vitamin C was shown in animal testing to reduce the effectiveness of the leukemia medication Bortezomib (Velcade®). Because of this risk, if taking these types of medications, supplements should be only be used after consulting with your doctor.
Because vitamin C improves the body's iron absorption, those suffering from hemochromatosis (pathological iron overload) should only use vitamin C supplements with regular monitoring from their doctor.
Vitamin B6, vitamin B12, and folic acid for high blood pressure
How it works
The body requires B vitamins to be able to break down homocysteine Homocysteine is a natural metabolic product which can damage the blood vessels if present in high levels. High homocysteine levels can promote the development of heart and circulatory disease, leading to stroke or heart attack. Vitamin B6, B12 and folic acid all help in the breakdown of homocysteine.
As shown in major observational studies, there is a direct correlation between folic acid intake and blood pressure levels. The risk of high blood pressure was also lower in the subjects with higher folic acid intake.
Folic acid, vitamin B6, and vitamin B12 deficiencies should always be counterbalanced with supplements to avoid high blood pressure.
Dosage and Recommended Use:
For effective reduction of homocysteine levels, 5 to 15 milligrams of vitamin B6, 400 to 600 micrograms of folic acid, and 250 to 500 micrograms of Vitamin B12 are recommended. B vitamins can be consumed via a multinutrient supplement, ideally combined with blood-vessel protecting antioxidants.
Tips
Active form of folic acid: Due to a genetic modification, approximately half of all people are unable or only partially able to convert folic acid into the active form required by the body. Make sure you take an active folic acid supplement - 5-Methyltetrahydrofolate (5-MTHF).
B vitamins can be consumed as a multinutrient supplement, ideally combined with the intake of blood-vessel protecting antioxidants.
Info
Exactly how B vitamins affect the possible consequences of high homocysteine levels, such as stroke and heart attacks, requires further study. Initial studies on this topic have produced positive results.
Testing homocysteine levels in the blood
The homocysteine levels in the blood should be tested to help avoid further damage to the blood vessels. Homocysteine testing is carried out on the blood plasma (the blood fluid without the blood cells). Normal levels are usually below 10 micromoles per liter.
B-vitamins: Instructions for pregnancy, when breastfeeding, while ill, or if taking medication
Vitamin B2, B6, and B12 should only be used in high dosages when pregnant or when breastfeeding if a deficiency has been confirmed and only after consultation with your gynecologist.
Diabetics with kidney damage and kidney patients must be particularly careful: do not take the cyanocobalamin form of vitamin B12 should not be used, but instead use methylcobalamin. High dosages of the vitamin cyanocobalamin are most likely harmful to patients with kidney problems.
The effects of using B vitamin supplements after the placement of a stent and after a heart attack have not been subject to a sufficient amount of study. B vitamins have a possible negative effect in these cases. High dosage vitamin B12 (60 to 400 micrograms per day) should be avoided.
At higher dosages (above 5 milligrams per day), vitamin B6 can reduce the effect of antiepileptic medications (Phenobarbital, Luminal®) und Phenytoin (Phenhydan®, Zentropil®) and medication for the treatment of Parkinson's disease (Levodopa (L-Dopa)). These active substances should not be taken in combination with high dose vitamin B6 supplements.
Dosage overview
Micronutrient medicine daily recommendation for high blood pressure
| Vitamins | |
|---|---|
| Vitamin D | 2000 to 4000 International Units (IU) |
| Vitamin C | 500 milligrams (mg) |
| Vitamin B6 | 5 to 15 milligrams (mg) |
| Vitamin B12 | 250 to 500 micrograms (µg) per day |
| Folic acid (5'-methyltetrahydrofolate) | 400 to 600 micrograms per day |
| Minerals | |
|---|---|
| Magnesium | 400 to 700 milligrams |
| Potassium | 2000 to 5000 milligrams |
| Other nutrients | |
|---|---|
| Taurine | 1500 to 4000 milligrams |
| Omega-3 fatty acids | 1500 to 2500 milligrams (with the highest possible EPA percentage) |
| Arginine | between 2000 and 6000 milligrams |
| Coenzyme Q10 | 200 milligrams |
| Bifidobacteria and Lactobacilli | at least 1 billion (109) bacteria |
Overview of recommended laboratory tests
Recommended blood tests for high blood pressure
| Normal reference range | |
|---|---|
| Magnesium | 1.38 to 1.50 Millimoles per liter (mmol/l) |
| Vitamin D | 40 to 60 nanograms per milliliter (ng/ml) |
| Arginine ratio ADMA:Arginine | between 100 and 300 Micromoles per liter (µmol/l) between 50:1 and 100:1 |
| Potassium | 3.6 to 4.8 Millimoles per liter |
| Homocysteine | below 10 micromoles per liter |
Supporting the effects of medication with micronutrients
ACE inhibitors bind zinc
ACE inhibitors containing the active pharmaceutical ingredients Captopril (Cor Tensobon®) or Enalapril (Xanef®) bind zinc in the body and boost its elimination. The long-term use of ACE inhibitors can lead to a zinc deficiency. Supplementing with 10 to 20 milligrams of zinc per day is advisable. However, both should not be taken at the same times to ensure that the zinc is not bound in the stomach before reaching the intestines.
Info
Zinc deficiency manifests itself through symptoms such as tiredness, hair loss, and difficulty healing wounds.
Beta blockers and angiotensin receptor blockers both cause deficiencies.
Beta blockers such as Metoprolol (like Lopressor®)disrupt the coenzyme Q10-dependent enzymes in the power plants of the cells - the mitochondria. Therefore, micronutritionists recommend at least 100 milligrams of coenzyme Q10 to ensure the energy supply of the heart muscle.
Angiotensin receptor blockers (Sartans), such as Losartan (Cozaar®) increase the amount of zinc being flushed out of the body. Especially during long-term treatment, there is a risk of developing a zinc deficiency because of this. Micronutritionists recommend supplementing 10 to 20 milligrams of zinc per day.
Diuretics flush out vitamins and minerals.
The typically prescribed diuretic for high blood pressure, with the active pharmaceutical ingredient hydrochlorothiazide (HCT), not only removes excess water from the body but also flushes out vitamins and minerals. These include B vitamins and the minerals zinc, magnesium, and potassium. Micronutritionists recommend daily:
- 200 to 400 micrograms of folic acid
- 5 to 15 milligrams Vitamin B6
- 100 to 200 micrograms of vitamin B12
- 10 to 20 milligrams of zinc
- 200 to 400 milligrams of magnesium
Example medications are Disalunil® or Esidrix®. There are many different combination supplements available; you can recognize them by the abbreviation HTC.
Dosage overview
Micronutrient recommendations when taking
| ACE inhibitors | |
|---|---|
| Zinc | 10 to 20 milligrams (mg) |
| Betablockers | |
|---|---|
| Coenzyme Q10 | at least 100 milligrams |
| Angiotensin receptor blockers | |
|---|---|
| Zinc | 10 to 20 milligrams |
| Diuretic medications | |
|---|---|
| Folic acid | 200 to 400 micrograms (µg) |
| Vitamin B6 | 5 to 15 milligrams |
| Vitamin B12 | 100 to 200 micrograms |
| Zinc | 10 to 20 milligrams |
| Magnesium | 200 to 400 milligrams |
Summary
Naturally reducing blood pressure levels with the help of micronutrient medicine: The nutrients magnesium, taurine, potassium, arginine and omega-3 fatty acids regulate the tension of the vascular muscles and therefore help determine the dilation of the blood vessels. This means there is more space in the vessels and the blood pressure level drops. Vitamin D regulates the production of the blood pressure hormone renin - this is why vitamin D deficiency increases the risk of high blood pressure. Also, scientists are currently investigating if an imbalance in the intestinal flora is related to high blood pressure levels. Further damage to the blood vessels can be prevented by supplementing antioxidants and B vitamins. Whether these supplements are also able to reduce high blood pressure levels will be determined in future studies.
Blood pressure medication can disrupt the micronutrient balance in the body: ACE inhibitors and angiotensin receptor blockers bind with zinc and remove it from the body. Diuretic medication also flushes micronutrients out of the body and deficiencies can develop. This is why micronutritionists recommend you also take zinc, magnesium, coenzyme Q10 or B vitamins.
Study and Source Index
Aburto, N.J. et al. (2013): Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013 Apr 3;346:f1378. https://www.ncbi.nlm.nih.gov/pubmed/23558164, retrieved on: 2017-10-30.
American Heart Association (2016): Fish and Omega-3 Fatty Acids http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/HealthyDietGoals/Fish-and-Omega-3-Fatty-Acids_UCM_303248_Article.jsp#.WYLrLYTyhhE, retrieved on: 2017-10-30.
aerzteblatt.de (2011): L-Arginin und Vitamine beugen Prä-Eklampsie vor. https://www.aerzteblatt.de/nachrichten/45939/L-Arginin-und-Vitamine-beugen-Prae-Eklampsie-vor, retrieved on: 2017-10-30.
Bischoff, S. C. (2009): Probiotika, Präbiotika und Synbiotika. 1. Aufl. Georg Thieme Verlag: Stuttgart, New York.
Colussi, G. et al. (2017): Impact of omega-3 polyunsaturated fatty acids on vascular function and blood pressure: Relevance for cardiovascular outcomes. Nutr Metab Cardiovasc Dis. 2017 Mar;27(3):191-200. https://www.ncbi.nlm.nih.gov/pubmed/27692558, retrieved on: 2017-10-30.
Dong, J.Y. et al. (2011): Effect of oral L-arginine supplementation on blood pressure: a meta-analysis of randomized, double-blind, placebo-controlled trials. Am Heart J. 2011 Dec;162(6):959-65. https://www.ncbi.nlm.nih.gov/pubmed/22137067, retrieved on: 2017-10-30.
Ellulu, M.S. et al. (2016): Effect of long chain omega-3 polyunsaturated fatty acids on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: a randomized controlled trial. Food Nutr Res. 2016 Jan 29;60:29268. https://www.ncbi.nlm.nih.gov/pubmed/26829184, retrieved on: 2017-10-30.
Filippini, T. et al. (2017): The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int J Cardiol.230:127-135. https://www.ncbi.nlm.nih.gov/pubmed/28024910, retrieved on: 2017-10-30.
Forman, J.P. et al. (2007): Plasma 25-hydroxyvitamin D levels and risk of incident hypertension. Hypertension. 2007 May;49(5):1063-9. https://www.ncbi.nlm.nih.gov/pubmed/17372031, retrieved on: 2017-10-30.
Gariballa, S.E. et al. (2012): Effects of mixed dietary supplements on total plasma homocysteine concentrations (tHcy): a randomized, double-blind, placebo-controlled trial. Int J Vitam Nutr Res. 82(4):260-6. https://www.ncbi.nlm.nih.gov/pubmed/23591663, retrieved on: 2017-10-30.
Gröber, U. (2011): Mikronährstoffe. Metabolic Tuning – Prävention – Therapie. 3. Aufl. Wissenschaftliche Verlagsgesellschaft mbH Stuttgart.
Gröber, U. (2014): Arzneimittel und Mikronährstoffe – Medikationsorientierte Supplementierung. 3. Aufl. Wissenschaftliche Verlagsgesellschaft mbH Stuttgart.
Harris, W.S. et al. (2017): The Omega-3 Index and relative risk for coronary heart disease mortality: Estimation from 10 cohort studies. Atherosclerosis. 262:51-54. https://www.ncbi.nlm.nih.gov/pubmed/28511049, retrieved on: 2017-10-30.
Hendijani, F. & Akbari, V. (2017): Probiotic supplementation for management of cardiovascular risk factors in adults with type II diabetes: A systematic review and meta-analysis. Clin Nutr. 2017 Feb 24. pii: S0261-5614(17)30065-1. https://www.ncbi.nlm.nih.gov/pubmed/28318686, retrieved on: 2017-10-30.
Herold, G. et al. (2017): Innere Medizin 2017. 1. Aufl. Gerd Herold, Köln.
Ho, M.J. et al. (2009): Blood pressure lowering efficacy of coenzyme Q10 for primary hypertension. Cochrane Database Syst Rev. 2009 Oct 7;(4):CD007435. https://www.ncbi.nlm.nih.gov/pubmed/19821418, retrieved on: 2017-10-30.
Houston, M. (2011): The Role of Magnesium in Hypertension and Cardiovascular Disease. J Clin Hypertens (Greenwich). 2011 Nov;13(11):843-7. https://www.ncbi.nlm.nih.gov/pubmed/22051430, retrieved on: 2017-10-30.
Huang, X. et al. (2017): Association between percent decline in serum total homocysteine and risk of first stroke. Neurology. 2017 Oct 13. https://www.ncbi.nlm.nih.gov/pubmed/29030456, retrieved on: 2017-10-30.
Juraschek, S.P. et al. (2012): Effects of vitamin C supplementation on blood pressure: a meta-analysis of randomized controlled trials. Am J Clin Nutr.95(5):1079-88. https://www.ncbi.nlm.nih.gov/pubmed/22492364, retrieved on: 2017-10-30.
Kass, L. et al. (2012): Effect of magnesium supplementation on blood pressure: a meta-analysis. Eur J Clin Nutr. 66(4):411-8. https://www.ncbi.nlm.nih.gov/pubmed/22318649, retrieved on: 2017-10-30.
Katakawa, M. et al. (2016): Taurine and magnesium supplementation enhances the function of endothelial progenitor cells through antioxidation in healthy men and spontaneously hypertensive rats. Hypertens Res. 2016 Dec;39(12):848-856. https://www.ncbi.nlm.nih.gov/pubmed/27412799, retrieved on: 2017-10-30.
Khalesi, S. et al. (2014): Effect of probiotics on blood pressure: a systematic review and meta-analysis of randomized, controlled trials. Hypertension. 2014 Oct;64(4):897-903. https://www.ncbi.nlm.nih.gov/pubmed/25047574, retrieved on: 2017-10-30.
Larsen, T. et al. (2012): Effect of cholecalciferol supplementation during winter months in patients with hypertension: a randomized, placebo-controlled trial. Am J Hypertens. 2012 Nov;25(11):1215-22. https://www.ncbi.nlm.nih.gov/pubmed/22854639, retrieved on: 2017-10-30.
McRae, M.P. et al. (2016): Therapeutic Benefits of l-Arginine: An Umbrella Review of Meta-analyses. J Chiropr Med. 2016 Sep;15(3):184-9. https://www.ncbi.nlm.nih.gov/pubmed/27660594, retrieved on: 2017-10-30.
Mehta, V. & Agarwal, S. (2017): Does Vitamin D Deficiency Lead to Hypertension? Cureus. 2017 Feb 17;9(2):e1038. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5356990, retrieved on: 2017-10-30.
Miller, P.E. et al. (2014): Long-chain omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid and blood pressure: a meta-analysis of randomized controlled trials. Am J Hypertens. 2014 Jul;27(7):885-96. https://www.ncbi.nlm.nih.gov/pubmed/24610882, retrieved on: 2017-10-30.
Minihane, A.M. et al. (2016): Consumption of Fish Oil Providing Amounts of Eicosapentaenoic Acid and Docosahexaenoic Acid That Can Be Obtained from the Diet Reduces Blood Pressure in Adults with Systolic Hypertension: A Retrospective Analysis. J Nutr. 2016 Mar;146(3):516-23. https://www.ncbi.nlm.nih.gov/pubmed/26817716, retrieved on: 2017-10-30.
Mohseni, M. et al. (2014): Effects of coenzyme q10 supplementation on serum lipoproteins, plasma fibrinogen, and blood pressure in patients with hyperlipidemia and myocardial infarction. Iran Red Crescent Med J. 2014 Oct 5;16(10):e16433. https://www.ncbi.nlm.nih.gov/pubmed/25763201, retrieved on: 2017-10-30.
Reule, C.A. et al. (2017): Effects of an L-arginine-based multi ingredient product on endothelial function in subjects with mild to moderate hypertension and hyperhomocysteinemia - a randomized, double-blind, placebo-controlled, cross-over trial. BMC Complement Altern Med. 2017 Feb 2;17(1):92. https://www.ncbi.nlm.nih.gov/pubmed/28153005, retrieved on: 2017-10-30.
Sun, Q. et al. (2016): Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension: Randomized, Double-Blind, Placebo-Controlled Study. Hypertension. 2016 Mar;67(3):541-9. https://www.ncbi.nlm.nih.gov/pubmed/26781281, retrieved on: 2017-10-30.
Thomas, G.N. et al. (2012): Vitamin D Levels Predict All-Cause and Cardiovascular Disease Mortality in Subjects With the Metabolic Syndrome. The Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Diabetes Care. 2012 May;35(5):1158-64. https://www.ncbi.nlm.nih.gov/pubmed/22399697, retrieved on: 2017-10-30.
Upadrasta, A. & Madempudi, R. S. (2016): Probiotics and blood pressure: current insights. Integr Blood Press Control. 2016; 9: 33–42. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4772943/, retrieved on: 2017-10-30.
Xuan, C. et al. (2016): Levels of asymmetric dimethylarginine (ADMA), an endogenous nitric oxide synthase inhibitor, and risk of coronary artery disease: A meta-analysis based on 4713 participants. Eur J Prev Cardiol. 2016 Mar;23(5):502-10. https://www.ncbi.nlm.nih.gov/pubmed/25956428, retrieved on: 2017-10-30.
Xun, P. et al. (2012): Folate intake and incidence of hypertension among American young adults: a 20-y follow-up study. Am J Clin Nutr. 95(5):1023-30. https://www.ncbi.nlm.nih.gov/pubmed/22492371, retrieved on: 2017-10-30.
Zhang, X. et al. (2016): Effects of Magnesium Supplementation on Blood Pressure: A Meta-Analysis of Randomized Double-Blind Placebo-Controlled Trials. Hypertension. 68(2):324-33. https://www.ncbi.nlm.nih.gov/pubmed/27402922, retrieved on: 2017-10-30.